We’re sorry, this site is currently experiencing technical difficulties. Please try again in a few moments. Exception: request blocked
Official websites use .gov
A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.

Increased Oropouche Virus Activity and Associated Risk to Travelers

Distributed via the CDC Health Alert Network August 16, 2024, 4:00 PM ET CDCHAN-00515
Summary The Centers for Disease Control and Prevention (CDC) is issuing this Health Alert Network (HAN) Health Advisory to notify clinicians and public health authorities of an increase in Oropouche virus disease in the Americas region, originating from endemic areas in the Amazon basin and new areas in South America and the Caribbean. Between January 1 and August 1, 2024, more than 8,000 cases of Oropouche virus disease were reported, including two deaths and five cases of vertical transmission associated with fetal death or congenital abnormalities. Countries reporting cases include Brazil, Bolivia, Peru, Colombia, and Cuba. In the United States and Europe in 2024, travel-associated cases have been identified in travelers returning from Cuba and Brazil. As testing and surveillance for Oropouche virus disease increase in the Americas, reports of cases from additional countries are expected. This Health Advisory advises on evaluating and testing travelers who have been in impacted areas with signs and symptoms consistent with Oropouche virus infection. It also raises awareness of the possible risk of vertical transmission (e.g., from gestational parent to fetus during pregnancy) and associated adverse effects on pregnancy and highlights prevention measures to mitigate additional spread of the virus and potential importation into unaffected areas, including the United States.
Background Oropouche virus belongs to the Simbu serogroup of the genus Orthobunyavirus in the Peribunyaviridae family. The virus was first detected in 1955 in Trinidad and Tobago and is endemic in the Amazon basin. Previous outbreaks have been described in Bolivia, Brazil, Colombia, Ecuador, French Guiana, Panama, and Peru. One child was infected in Haiti in 2014. The current 2024 outbreak is occurring in endemic areas and new areas outside the Amazon basin; countries reporting locally acquired (autochthonous) cases include Brazil, Bolivia, Peru, Colombia, and Cuba. Although travel-associated cases have been identified in the United States (n=11), no evidence of local transmission currently exists within the United States or its territories.
Sylvatic (enzootic) transmission of Oropouche virus occurs in forested areas between mosquitoes and non-human vertebrate hosts (e.g., sloths, non-human primates, domestic and wild birds, and rodents). Humans can become infected while visiting forested areas and are likely responsible for introducing the virus into urban environments. Humans contribute to the transmission cycle in urban environments since infected humans develop sufficient viremia to serve as amplifying hosts. Biting midges ( Culicoides paraensis ) and possibly certain mosquitoes ( Culex quinquefasciatus) are responsible for transmitting the virus from an infected person to an uninfected person in urban areas.
Approximately 60% of people infected with Oropouche virus become symptomatic . The incubation period is typically 3–10 days. Initial clinical presentation is similar to diseases caused by dengue , Zika , and chikungunya viruses, with acute onset of fever, chills, headache, myalgia, and arthralgia. Other symptoms can include retroorbital (eye) pain, photophobia (light sensitivity), nausea, vomiting, diarrhea, fatigue, maculopapular rash,conjunctival injection, and abdominal pain. Clinical laboratory findings can include lymphopenia and leukopenia, elevated C-reactive protein (CRP), and slightly elevated liver enzymes. Initial symptoms typically resolve after a few days, but a high proportion (about 70%) experience recurrent symptoms days to weeks after resolution of their initial illness. Although illness is typically mild, it is estimated less than 5% of patients can develop hemorrhagic manifestations (e.g., epistaxis, gingival bleeding, melena, menorrhagia, petechiae) or neuroinvasive disease (e.g., meningitis, meningoencephalitis). Neuroinvasive disease symptoms may include intense occipital pain, dizziness, confusion, lethargy, photophobia, nausea, vomiting, nuchal rigidity, and nystagmus. Clinical laboratory findings for patients with neuroinvasive disease include pleocytosis and elevated protein in cerebrospinal fluid (CSF).
Although people exposed to biting midges or mosquitoes infected with the virus are most at risk for developing disease, the risk factors for more severe Oropouche virus disease are not well-defined. People at risk for more severe disease likely include those at risk for severe disease with other viral infections transmitted by vectors (e.g., people aged 65 years or older, or those with underlying medical conditions, such as immune suppression, hypertension, diabetes, or cardiovascular disease). Earlier this year, Brazil reported two deaths in otherwise healthy non-pregnant women, and five cases in pregnant people with evidence of vertical transmission of the virus to the fetus associated with fetal death or congenital abnormalities, including microcephaly. This was the first report of deaths and Oropouche virus vertical transmission and associated adverse birth outcomes.
Laboratory diagnosis is generally accomplished by testing serum. Cerebrospinal fluid can also be tested in patients with signs and symptoms of neuroinvasive disease. Diagnostic testing is available at some public health laboratories (e.g., Wadsworth Center, NYS Department of Health) and at CDC. CDC and other public health laboratories are currently working to validate additional diagnostic assays. Contact your state, tribal, local, or territorial health department for more information and to facilitate testing. For current testing and case reporting guidance, visit CDC’s website . In many countries, outbreaks of dengue are occurring in areas with reported Oropouche virus transmission. For patients with suspected Oropouche virus disease, it is important to rule out dengue virus infection because proper clinical management of dengue can improve health outcomes. Other diagnostic considerations include chikungunya, Zika, leptospirosis, malaria, or infections caused by various other bacterial or viral pathogens (e.g., rickettsia, group A streptococcus, rubella, measles, parvovirus, enteroviruses, adenovirus, Mayaro virus).
No specific antiviral treatments or vaccines are available for Oropouche virus disease. Treatment for symptoms can include rest, fluids, and use of analgesics and antipyretics. Acetaminophen is the preferred first-line treatment for fever and pain. Aspirin and other non-steroidal anti-inflammatory drugs (NSAIDs) should not be used to reduce the risk of hemorrhage. Patients who develop more severe symptoms should be hospitalized for close observation and supportive treatment. Pregnant people with laboratory evidence of Oropouche virus infection should be monitored during pregnancy and live-born infants should be carefully evaluated.
Travelers to areas with Oropouche virus transmission should use prevention measures to avoid biting midge and mosquito exposure during travel and for 3 weeks after travel, or if infected during the first week of illness, to mitigate additional spread of the virus and potential importation into unaffected areas in the United States. Oropouche virus disease is not a nationally notifiable condition. However, CDC encourages jurisdictions to report voluntarily to ArboNET , the national arboviral disease surveillance system.
Recommendations for Healthcare Providers
- Abrupt onset of reported fever, headache, and one or more of the following: myalgia, arthralgia, photophobia, retroorbital/eye pain, or signs and symptoms of neuroinvasive disease (e.g., stiff neck, altered mental status, seizures, limb weakness, or cerebrospinal fluid pleocytosis); AND
- No respiratory symptoms (e.g., cough, rhinorrhea, shortness of breath); AND
- Tested negative for other possible diseases, in particular dengue. If strong suspicion of Oropouche virus disease exists based on the patient’s clinical features and history of travel to an area with virus circulation, do not wait for negative testing for other infections before contacting your state, tribal, local, or territorial health department.
- Contact your state, tribal, local, or territorial health department to facilitate diagnostic testing.
- Rule out dengue virus infection in travelers with suspect Oropouche virus infection because these viruses often cocirculate and cause similar clinical presentations during acute illness. Early clinical management of dengue can improve health outcomes.
- Be aware that a high proportion of patients (about 70%) with Oropouche virus disease may experience recurrent symptoms days to weeks after resolution of their initial illness.
- Be aware of the risk of vertical transmission and possible adverse impacts on the fetus, including fetal death or congenital abnormalities. Monitor pregnancies in people with laboratory evidence of Oropouche virus infection and provide thorough infant evaluations.
- Inform pregnant people of the possible risks to the fetus when considering travel to areas with reported Oropouche virus transmission. Counsel these patients to consider the destination, reason for traveling, and their ability to prevent insect bites.
- Pregnant people are currently recommended to reconsider non-essential travel to areas with an Oropouche virus Level 2 Travel Health Notice . If a pregnant person decides to travel, counsel them to strictly prevent insect bites during travel.
- Manage travelers with suspect Oropouche virus disease with acetaminophen as the preferred first-line treatment for fever and pain. Aspirin and other NSAIDS should not be used to reduce the risk of hemorrhage.
- Be aware that people who may be at higher risk for complications or severe disease include pregnant people, older adults (e.g., aged 65 years or older), and people with underlying medical conditions (e.g., immune suppression, hypertension, diabetes, or cardiovascular disease).
- Direct all travelers going to areas with Oropouche virus transmission to use measures to prevent insect bites during travel and for 3 weeks after travel, or if infected, during the first week of illness to mitigate additional spread of the virus and potential importation into unaffected areas in the United States.
- Report all suspected Oropouche virus disease infections to your state, tribal, local, or territorial health department to facilitate diagnosis and mitigate risk of local transmission. For after-hours contact information for health departments please visit: https://www.cste.org/page/EpiOnCall . Please follow standard procedures for reporting during normal business hours.
Recommendations for Health Departments
- Share Oropouche virus prevention messages for travelers and pregnant persons with healthcare providers, travel health clinics and the public.
- Perform surveillance for Oropouche virus disease cases in travelers who have been in areas with Oropouche virus transmission and be aware of risk of possible local transmission in areas where biting midges ( Culicoides paraensis) and mosquitoes ( Culex quinquefasciatus) are currently active.
- Keep current on CDC’s evolving testing and case reporting guidance .
- Assist healthcare providers with obtaining appropriate testing for diagnosing Oropouche virus infection.
- Voluntarily report confirmed and probable Oropouche virus infections to CDC via ArboNET , the national surveillance system for arthropod-borne viruses.
- Contact CDC ( [email protected] ) if concern exists for local transmission in a non-endemic area. Consider if the patient had contact with a person with confirmed Oropouche virus infection, lives in an area where travel-related cases have been identified, or has known vector exposure (e.g., mosquitoes or biting midges).
Recommendations for Travelers
- All travelers can protect themselves from Oropouche, dengue, Zika, and other viruses transmitted by insects by preventing insect bites , including using an Environmental Protection Agency (EPA)-registered insect repellent ; wearing long-sleeved shirts and pants; and staying in places with air conditioning or that use window and door screens.
- Pregnant travelers should discuss travel plans, reasons for travel, steps to prevent insect bites, and potential risk with their healthcare provider.
- Pregnant people considering travel to countries with an Oropouche virus Level 2 Travel Health Notice should reconsider non-essential travel. If travel is unavoidable, pregnant travelers should strictly follow Oropouche virus prevention recommendations to prevent insect bites during travel.
- Travelers should be aware that the most common symptoms of Oropouche virus are fever and headache and that symptoms usually begin 3-10 days after being bitten by an infected midge or mosquito. Most people infected with Oropouche virus feel better within a week, but symptoms often come back.
- Travelers who have been in areas with Oropouche virus transmission should prevent insect bites for 3 weeks after travel.
- Seek medical care and tell their healthcare provider when and where they traveled.
- Not take aspirin or other NSAIDS (e.g., ibuprofen) to reduce the risk of bleeding.
- Continue to prevent insect bites during the first week of illness to avoid further spread, especially in areas where mosquitoes or biting midges are active.
For More Information
- About Oropouche | CDC
- Travel Health Notices| CDC
- Preventing Mosquito Bites | CDC
- Find the Repellent that is Right for You | EPA
- Dengue: Guidelines for Diagnosis, Treatment, Prevention and Control | WHO
- The Lancet Infectious Diseases. Oropouche fever, the mysterious threat. Lancet Infect Dis. 2024 Aug 8:S1473-3099(24)00516-4. doi: 10.1016/S1473-3099(24)00516-4. Epub ahead of print.
- Pan American Health Organization / World Health Organization. Epidemiological Alert: Oropouche in the Region of the Americas: vertical transmission event under investigation in Brazil, 17 July 2024 . Washington, D.C.; 2024.
- Pan American Health Organization / World Health Organization. Epidemiological Alert: Oropouche in the Region of the Americas, 1 August 2024 . Washington, D.C.; 2024.
- Florida Department of Health. Florida arbovirus surveillance Week 31: August 4-August 10, 2024. https://www.floridahealth.gov/diseases-and-conditions/mosquito-borne-diseases/surveillance.html .
- European Centre for Disease Prevention and Control. Oropouche virus disease cases imported into the European Union – 9 August 2024 . Stockholm; 2024.
- Ladner JT, Savji N, Lofts L, et al. Genomic and phylogenetic characterization of viruses included in the Manzanilla and Oropouche species complexes of the genus Orthobunyavirus, family Bunyaviridae . J Gen Virol . 2014 May; 95(Pt 5):1055-1066. doi: 10.1099/vir.0.061309-0.
- Pinheiro FP, Travassos da Rosa AP, Travassos da Rosa JF, et al. Oropouche virus. I. A review of clinical, epidemiological, and ecological findings . Am J Trop Med Hyg. 1981; 30(1):149-60.
- Pinheiro FP, Travassos da Rosa AP, Gomes ML, et al. Transmission of Oropouche virus from man to hamster by the midge Culicoides paraensis . Science . 1982; 215(4537):1251-3. doi: 10.1126/science.6800036.
- Roberts DR, Hoch AL, Dixon KE, et al. Oropouche virus. III. Entomological observations from three epidemics in Pará, Brazil, 1975. Am J Trop Med Hyg . 1981; 30(1):165-71.
- Cardoso BF, Serra OP, Heinen LB, et al. Detection of Oropouche virus segment S in patients and in Culex quinquefasciatus in the state of Mato Grosso, Brazil. Mem Inst Oswaldo Cruz . 2015; 110(6):745-54. doi: 10.1590/0074-02760150123.
- Pan American Health Organization / World Health Organization. Public Health Risk Assessment related to Oropouche Virus (OROV) in the Region of the Americas, 3 August 2024. Washington, D.C.; 2024.
The Centers for Disease Control and Prevention (CDC) protects people’s health and safety by preventing and controlling diseases and injuries; enhances health decisions by providing credible information on critical health issues; and promotes healthy living through strong partnerships with local, national and international organizations.
Department of Health and Human Services
Han message types.
- Health Alert: Conveys the highest level of importance about a public health incident.
- Health Advisory: Provides important information about a public health incident.
- Health Update: Provides updated information about a public health incident.
### This message was distributed to state and local health officers, state and local epidemiologists, state and local laboratory directors, public information officers, HAN coordinators, and clinician organizations. ###
- HAN Archive By Year
- Sign Up for HAN Email Updates
- HAN Jurisdictions
- Prepare Your Health
- Coping with a Disaster or Traumatic Event
- Information on Specific Types of Emergencies
- Information for Specific Groups
- Resources for Emergency Health Professionals
- Training & Education
- Social Media
- Preparation & Planning
- What CDC is Doing
- Blog: Public Health Matters

Security Alert May 17, 2024
Worldwide caution.
- Travel Advisories |
- Contact Us |
- MyTravelGov |
Find U.S. Embassies & Consulates
Travel.state.gov, congressional liaison, special issuance agency, u.s. passports, international travel, intercountry adoption, international parental child abduction, records and authentications, popular links, travel advisories, mytravelgov, stay connected, legal resources, legal information, info for u.s. law enforcement, replace or certify documents.
Share this page:
Learn about your destination
Take 90 seconds for safer travel.
Travel Advisory Levels
Enroll in step.

Subscribe to get up-to-date safety and security information and help us reach you in an emergency abroad.
Recommended Web Browsers: Microsoft Edge or Google Chrome.
External Link
You are about to leave travel.state.gov for an external website that is not maintained by the U.S. Department of State.
Links to external websites are provided as a convenience and should not be construed as an endorsement by the U.S. Department of State of the views or products contained therein. If you wish to remain on travel.state.gov, click the "cancel" message.
You are about to visit:
Advertisement
Supported by
What to Know About the C.D.C. Guidelines on Vaccinated Travel
In updated recommendations, the federal health agency said both domestic and international travel was low risk for fully vaccinated Americans. But travel remains far from simple.
- Share full article

By Ceylan Yeginsu
The Centers for Disease Control and Prevention updated its guidance for fully vaccinated Americans in April, saying that traveling both domestically and internationally was low risk.
The long-awaited recommendations were issued by federal health officials after a series of studies found that vaccines administered in the United States were robustly effective in preventing infections in real-life conditions.
One is considered fully vaccinated two weeks after receiving the single dose of the Johnson & Johnson vaccine, or two weeks after receiving the second dose of the Pfizer-BioNTech or Moderna shots.
If you decide to travel, you might still have some questions. Here are the answers.
Will I still need to wear a mask and socially distance while traveling?
Yes. Under federal law, masks must be worn at airports in the United States, onboard domestic flights and in all transport hubs. The C.D.C. says that as long as coronavirus measures are taken in these scenarios, including mask wearing, fully vaccinated Americans can travel domestically without having to take a test or quarantine, although the agency warns that some states and territories may keep their local travel restrictions and recommendations in place.
For those wishing to travel internationally, a coronavirus test will not be required before departure from the United States unless mandated by the government of their destination. Vaccinated travelers are still required to get tested three days before travel by air into the United States, and are advised to take a test three to five days after their return, but will not need to self-quarantine.
Can I go abroad?
Yes, but only to countries that will have you.
More than half the world’s countries have reopened to tourists from the United States, including the countries of the European Union , which on June 18 added the United States to its “safe list” of countries, meaning that American travelers can now visit. While the European Union aims to take a coordinated approach to travel this summer, member states will be allowed to set their own requirements for travelers from individual countries based on their own epidemiological criteria, which means they may require testing or vaccination.
Some places like Turkey, Croatia and Montenegro had already been welcoming Americans with negative test results. Greece joined that growing list in May, ahead of most European countries, opening to fully vaccinated tourists and other foreigners with a negative test.
Many Caribbean nations have reopened to American tourists, but each has its own coronavirus protocols and entry requirements.
Here’s a full list of countries Americans can currently travel to.
What about domestic travel? Is it free and clear to cross state borders?
If you are fully vaccinated, the C.D.C. says you can travel freely within the United States and that you do not need to get tested, or self-quarantine, before or after traveling. But some states and local governments may choose to keep travel restrictions in place, including testing, quarantine and stay-at-home orders. Hawaii , for instance, still has travel restrictions in place.
Before you travel across state lines, check the current rules at your destination.
How are they going to check that I’m fully vaccinated?
Right now, the best way to prove that you have been vaccinated is to show your vaccine card .
Digital vaccine and health certificates showing that people have been vaccinated or tested are in various stages of development around the world and are expected, eventually, to be widely used to speed up travel.
The subject of “ vaccine passports ” is currently one of the most hotly debated topics within the travel industry, with questions over the equity of their use and concerns over health and data privacy.
In early April, Gov. Ron DeSantis of Florida issued an executive order that would ban local governments and state businesses from requiring proof of vaccination for services.
And in March, the European Union endorsed its own vaccine certificate , which some countries are already using, with more expected to adopt it by July 1.
But what about my kids? What’s the guidance on traveling with unvaccinated people?
The C.D.C. advises people against travel unless they have been vaccinated. If you must travel, the agency recommends testing one to three days before a trip and following all coronavirus guidance at your destination.
In May, the F.D.A. expanded its emergency use authorization of the Pfizer-BioNTech coronavirus vaccine to include adolescents between 12 and 15 years of age.
All air passengers aged two and older coming into the United States, including fully vaccinated people, are required to have a negative Covid-19 test result taken no more than three days before they board their flight.
What is my moral obligation to the places I visit where most people are not vaccinated?
The United States inoculation rollout has been among the fastest in the world, but there is a stark gap between its rapid rollout and the vaccination programs in different countries. Some nations have yet to report a single dose being administered.
Many countries are currently seeing a surge in new cases and are implementing strict coronavirus protocols, including mask mandates in public spaces, capacity limits at restaurants and tourist sites and other lockdown restrictions.
It is important to check coronavirus case rates, measures and medical infrastructure before traveling to your destination and not to let your guard down when you get there. Even though you are fully vaccinated, you may still be able to transmit the disease to local communities who have not yet been inoculated.
You can track coronavirus vaccination rollouts around the world here.
Follow New York Times Travel on Instagram , Twitter and Facebook . And sign up for our weekly Travel Dispatch newsletter to receive expert tips on traveling smarter and inspiration for your next vacation.
Ceylan Yeginsu is a London-based reporter. She joined The Times in 2013, and was previously a correspondent in Turkey covering politics, the migrant crisis, the Kurdish conflict, and the rise of Islamic State extremism in Syria and the region. More about Ceylan Yeginsu
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- About COVID-19
- People with Certain Medical Conditions and COVID-19
- COVID-19 Vaccines
- How to Protect Yourself and Others
- Tools and Resources
- View All Home
- Clinical Care
- Infection Control Guidance
- Clinical Care Quick Reference
- Overview of Testing for SARS-CoV-2
- Containing COVID-19 in Non-U.S. Healthcare Settings
- Surveillance and Data Analytics
- Safety Precautions: Cleaning and Disinfecting for COVID-19
- Interim Guidelines for Biosafety and COVID-19
- CDC Science behind Long COVID
- Health Equity in COVID-19
- Variants and Genomic Surveillance for SARS-CoV-2
Coronavirus Disease 2019 (COVID-19)
Español

For Professionals
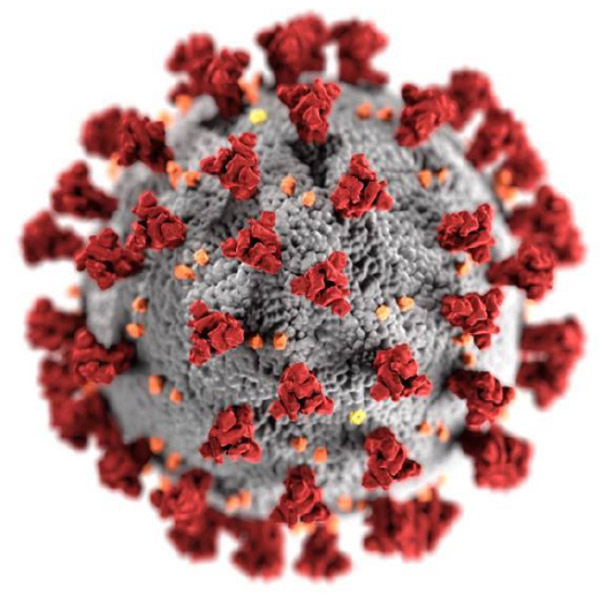
COVID-19 (coronavirus disease 2019) is a disease caused by a virus named SARS-CoV-2. It can be very contagious and spreads quickly.
For Everyone
Health care providers, public health.
You are using an outdated browser. Upgrade your browser today or install Google Chrome Frame to better experience this site.
Uganda Traveler View
Travel health notices, vaccines and medicines, non-vaccine-preventable diseases, stay healthy and safe.
- Packing List
After Your Trip

Be aware of current health issues in Uganda. Learn how to protect yourself.
Level 2 Practice Enhanced Precautions
- Updated Global Polio August 20, 2024 Some international destinations have circulating poliovirus. Before any international travel, make sure you are up to date on your polio vaccines. Destination List: Afghanistan, Algeria, Angola, Benin, Botswana, Burkina Faso, Burundi, Cameroon, Central African Republic, Chad, Côte d'Ivoire (Ivory Coast), Democratic Republic of the Congo, Egypt, Ethiopia, Guinea, Indonesia, Kenya, Liberia, Madagascar, Mali, Mauritania, Mozambique, Niger, Nigeria, Pakistan, Republic of South Sudan, Republic of the Congo, Senegal, Sierra Leone, Somalia, Sudan, Tanzania, including Zanzibar, The Gambia, Uganda, Yemen, Zambia, Zimbabwe
- Clade I Mpox in the Democratic Republic of the Congo and Neighboring Countries August 07, 2024 There is an outbreak of clade I mpox in the Democratic Republic of the Congo (DRC). Countries sharing borders with DRC are considered at risk for spread. Destination List: Burundi, Central African Republic, Democratic Republic of the Congo, Republic of the Congo, Rwanda, Uganda
⇧ Top
Check the vaccines and medicines list and visit your doctor at least a month before your trip to get vaccines or medicines you may need. If you or your doctor need help finding a location that provides certain vaccines or medicines, visit the Find a Clinic page.
- Avoid contaminated water
Leptospirosis
How most people get sick (most common modes of transmission)
- Touching urine or other body fluids from an animal infected with leptospirosis
- Swimming or wading in urine-contaminated fresh water, or contact with urine-contaminated mud
- Drinking water or eating food contaminated with animal urine
- Avoid contaminated water and soil
- Avoid floodwater
Clinical Guidance
Schistosomiasis
- Wading, swimming, bathing, or washing in contaminated freshwater streams, rivers, ponds, lakes, or untreated pools.
Avoid bug bites
African sleeping sickness (african trypanosomiasis).
- Tsetse fly bite
- Avoid Bug Bites
African Trypanosomiasis
African Tick-Bite Fever
African Tick-bite fever
Chikungunya
- Mosquito bite
Crimean-Congo Hemorrhagic fever
- Tick bite
- Touching the body fluids of a person or animal infected with CCHF
- Mosquito bite
- An infected pregnant woman can spread it to her unborn baby
- Avoid animals
- Touching infected animals (including bats and primates) or their body fluids
- Touching body fluids (blood or sweat) from an infected person
- Touching objects contaminated with the body fluids of a person infected with Ebola or Marburg virus
- Avoid sick people
- Avoid animals and areas where they live
Ebola virus
Marburg Hemorrhagic Fever
Marburg virus
Rift Valley Fever
- Touching blood, body fluids, or tissue of infected livestock
Rift Valley fever
Airborne & droplet
- Breathing in air or accidentally eating food contaminated with the urine, droppings, or saliva of infected rodents
- Bite from an infected rodent
- Less commonly, being around someone sick with hantavirus (only occurs with Andes virus)
- Avoid rodents and areas where they live
Tuberculosis (TB)
- Breathe in TB bacteria that is in the air from an infected and contagious person coughing, speaking, or singing.
Learn actions you can take to stay healthy and safe on your trip. Vaccines cannot protect you from many diseases in Uganda, so your behaviors are important.
Eat and drink safely
Food and water standards around the world vary based on the destination. Standards may also differ within a country and risk may change depending on activity type (e.g., hiking versus business trip). You can learn more about safe food and drink choices when traveling by accessing the resources below.
- Choose Safe Food and Drinks When Traveling
- Water Treatment Options When Hiking, Camping or Traveling
- Global Water, Sanitation and Hygiene (WASH)
- Avoid Contaminated Water During Travel
You can also visit the Department of State Country Information Pages for additional information about food and water safety.
Prevent bug bites
Bugs (like mosquitoes, ticks, and fleas) can spread a number of diseases in Uganda. Many of these diseases cannot be prevented with a vaccine or medicine. You can reduce your risk by taking steps to prevent bug bites.
What can I do to prevent bug bites?
- Cover exposed skin by wearing long-sleeved shirts, long pants, and hats.
- Use an appropriate insect repellent (see below).
- Use permethrin-treated clothing and gear (such as boots, pants, socks, and tents). Do not use permethrin directly on skin.
- Stay and sleep in air-conditioned or screened rooms.
- Use a bed net if the area where you are sleeping is exposed to the outdoors.
What type of insect repellent should I use?
- FOR PROTECTION AGAINST TICKS AND MOSQUITOES: Use a repellent that contains 20% or more DEET for protection that lasts up to several hours.
- Picaridin (also known as KBR 3023, Bayrepel, and icaridin)
- Oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD)
- 2-undecanone
- Always use insect repellent as directed.
What should I do if I am bitten by bugs?
- Avoid scratching bug bites, and apply hydrocortisone cream or calamine lotion to reduce the itching.
- Check your entire body for ticks after outdoor activity. Be sure to remove ticks properly.
What can I do to avoid bed bugs?
Although bed bugs do not carry disease, they are an annoyance. See our information page about avoiding bug bites for some easy tips to avoid them. For more information on bed bugs, see Bed Bugs .
For more detailed information on avoiding bug bites, see Avoid Bug Bites .
Stay safe outdoors
If your travel plans in Uganda include outdoor activities, take these steps to stay safe and healthy during your trip.
- Stay alert to changing weather conditions and adjust your plans if conditions become unsafe.
- Prepare for activities by wearing the right clothes and packing protective items, such as bug spray, sunscreen, and a basic first aid kit.
- Consider learning basic first aid and CPR before travel. Bring a travel health kit with items appropriate for your activities.
- If you are outside for many hours in heat, eat salty snacks and drink water to stay hydrated and replace salt lost through sweating.
- Protect yourself from UV radiation : use sunscreen with an SPF of at least 15, wear protective clothing, and seek shade during the hottest time of day (10 a.m.–4 p.m.).
- Be especially careful during summer months and at high elevation. Because sunlight reflects off snow, sand, and water, sun exposure may be increased during activities like skiing, swimming, and sailing.
- Very cold temperatures can be dangerous. Dress in layers and cover heads, hands, and feet properly if you are visiting a cold location.
Stay safe around water
- Swim only in designated swimming areas. Obey lifeguards and warning flags on beaches.
- Practice safe boating—follow all boating safety laws, do not drink alcohol if driving a boat, and always wear a life jacket.
- Do not dive into shallow water.
- Do not swim in freshwater in developing areas or where sanitation is poor.
- Avoid swallowing water when swimming. Untreated water can carry germs that make you sick.
- To prevent infections, wear shoes on beaches where there may be animal waste.
Schistosomiasis, a parasitic infection that can be spread in fresh water, is found in Uganda. Avoid swimming in fresh, unchlorinated water, such as lakes, ponds, or rivers.
Keep away from animals
Most animals avoid people, but they may attack if they feel threatened, are protecting their young or territory, or if they are injured or ill. Animal bites and scratches can lead to serious diseases such as rabies.
Follow these tips to protect yourself:
- Do not touch or feed any animals you do not know.
- Do not allow animals to lick open wounds, and do not get animal saliva in your eyes or mouth.
- Avoid rodents and their urine and feces.
- Traveling pets should be supervised closely and not allowed to come in contact with local animals.
- If you wake in a room with a bat, seek medical care immediately. Bat bites may be hard to see.
All animals can pose a threat, but be extra careful around dogs, bats, monkeys, sea animals such as jellyfish, and snakes. If you are bitten or scratched by an animal, immediately:
- Wash the wound with soap and clean water.
- Go to a doctor right away.
- Tell your doctor about your injury when you get back to the United States.
Consider buying medical evacuation insurance. Rabies is a deadly disease that must be treated quickly, and treatment may not be available in some countries.
Reduce your exposure to germs
Follow these tips to avoid getting sick or spreading illness to others while traveling:
- Wash your hands often, especially before eating.
- If soap and water aren’t available, clean hands with hand sanitizer (containing at least 60% alcohol).
- Don’t touch your eyes, nose, or mouth. If you need to touch your face, make sure your hands are clean.
- Cover your mouth and nose with a tissue or your sleeve (not your hands) when coughing or sneezing.
- Try to avoid contact with people who are sick.
- If you are sick, stay home or in your hotel room, unless you need medical care.
Avoid sharing body fluids
Diseases can be spread through body fluids, such as saliva, blood, vomit, and semen.
Protect yourself:
- Use latex condoms correctly.
- Do not inject drugs.
- Limit alcohol consumption. People take more risks when intoxicated.
- Do not share needles or any devices that can break the skin. That includes needles for tattoos, piercings, and acupuncture.
- If you receive medical or dental care, make sure the equipment is disinfected or sanitized.
Know how to get medical care while traveling
Plan for how you will get health care during your trip, should the need arise:
- Carry a list of local doctors and hospitals at your destination.
- Review your health insurance plan to determine what medical services it would cover during your trip. Consider purchasing travel health and medical evacuation insurance.
- Carry a card that identifies, in the local language, your blood type, chronic conditions or serious allergies, and the generic names of any medications you take.
- Some prescription drugs may be illegal in other countries. Call Uganda’s embassy to verify that all of your prescription(s) are legal to bring with you.
- Bring all the medicines (including over-the-counter medicines) you think you might need during your trip, including extra in case of travel delays. Ask your doctor to help you get prescriptions filled early if you need to.
Many foreign hospitals and clinics are accredited by the Joint Commission International. A list of accredited facilities is available at their website ( www.jointcommissioninternational.org ).
In some countries, medicine (prescription and over-the-counter) may be substandard or counterfeit. Bring the medicines you will need from the United States to avoid having to buy them at your destination.
Malaria is a risk in Uganda. Fill your malaria prescription before you leave and take enough with you for the entire length of your trip. Follow your doctor’s instructions for taking the pills; some need to be started before you leave.
Select safe transportation
Motor vehicle crashes are the #1 killer of healthy US citizens in foreign countries.
In many places cars, buses, large trucks, rickshaws, bikes, people on foot, and even animals share the same lanes of traffic, increasing the risk for crashes.
Be smart when you are traveling on foot.
- Use sidewalks and marked crosswalks.
- Pay attention to the traffic around you, especially in crowded areas.
- Remember, people on foot do not always have the right of way in other countries.

Riding/Driving
Choose a safe vehicle.
- Choose official taxis or public transportation, such as trains and buses.
- Ride only in cars that have seatbelts.
- Avoid overcrowded, overloaded, top-heavy buses and minivans.
- Avoid riding on motorcycles or motorbikes, especially motorbike taxis. (Many crashes are caused by inexperienced motorbike drivers.)
- Choose newer vehicles—they may have more safety features, such as airbags, and be more reliable.
- Choose larger vehicles, which may provide more protection in crashes.
Think about the driver.
- Do not drive after drinking alcohol or ride with someone who has been drinking.
- Consider hiring a licensed, trained driver familiar with the area.
- Arrange payment before departing.
Follow basic safety tips.
- Wear a seatbelt at all times.
- Sit in the back seat of cars and taxis.
- When on motorbikes or bicycles, always wear a helmet. (Bring a helmet from home, if needed.)
- Avoid driving at night; street lighting in certain parts of Uganda may be poor.
- Do not use a cell phone or text while driving (illegal in many countries).
- Travel during daylight hours only, especially in rural areas.
- If you choose to drive a vehicle in Uganda, learn the local traffic laws and have the proper paperwork.
- Get any driving permits and insurance you may need. Get an International Driving Permit (IDP). Carry the IDP and a US-issued driver's license at all times.
- Check with your auto insurance policy's international coverage, and get more coverage if needed. Make sure you have liability insurance.
- Avoid using local, unscheduled aircraft.
- If possible, fly on larger planes (more than 30 seats); larger airplanes are more likely to have regular safety inspections.
- Try to schedule flights during daylight hours and in good weather.
Medical Evacuation Insurance
If you are seriously injured, emergency care may not be available or may not meet US standards. Trauma care centers are uncommon outside urban areas. Having medical evacuation insurance can be helpful for these reasons.
Helpful Resources
Road Safety Overseas (Information from the US Department of State): Includes tips on driving in other countries, International Driving Permits, auto insurance, and other resources.
The Association for International Road Travel has country-specific Road Travel Reports available for most countries for a minimal fee.
Traffic flows on the left side of the road in Uganda.
- Always pay close attention to the flow of traffic, especially when crossing the street.
- LOOK RIGHT for approaching traffic.
Maintain personal security
Use the same common sense traveling overseas that you would at home, and always stay alert and aware of your surroundings.
Before you leave
- Research your destination(s), including local laws, customs, and culture.
- Monitor travel advisories and alerts and read travel tips from the US Department of State.
- Enroll in the Smart Traveler Enrollment Program (STEP) .
- Leave a copy of your itinerary, contact information, credit cards, and passport with someone at home.
- Pack as light as possible, and leave at home any item you could not replace.
While at your destination(s)
- Carry contact information for the nearest US embassy or consulate .
- Carry a photocopy of your passport and entry stamp; leave the actual passport securely in your hotel.
- Follow all local laws and social customs.
- Do not wear expensive clothing or jewelry.
- Always keep hotel doors locked, and store valuables in secure areas.
- If possible, choose hotel rooms between the 2nd and 6th floors.
Healthy Travel Packing List
Use the Healthy Travel Packing List for Uganda for a list of health-related items to consider packing for your trip. Talk to your doctor about which items are most important for you.
Why does CDC recommend packing these health-related items?
It’s best to be prepared to prevent and treat common illnesses and injuries. Some supplies and medicines may be difficult to find at your destination, may have different names, or may have different ingredients than what you normally use.
If you are not feeling well after your trip, you may need to see a doctor. If you need help finding a travel medicine specialist, see Find a Clinic . Be sure to tell your doctor about your travel, including where you went and what you did on your trip. Also tell your doctor if you were bitten or scratched by an animal while traveling.
If your doctor prescribed antimalarial medicine for your trip, keep taking the rest of your pills after you return home. If you stop taking your medicine too soon, you could still get sick.
Malaria is always a serious disease and may be a deadly illness. If you become ill with a fever either while traveling in a malaria-risk area or after you return home (for up to 1 year), you should seek immediate medical attention and should tell the doctor about your travel history.
For more information on what to do if you are sick after your trip, see Getting Sick after Travel .
Map Disclaimer - The boundaries and names shown and the designations used on maps do not imply the expression of any opinion whatsoever on the part of the Centers for Disease Control and Prevention concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Approximate border lines for which there may not yet be full agreement are generally marked.
Other Destinations
If you need help finding travel information:
Message & data rates may apply. CDC Privacy Policy
File Formats Help:
- Adobe PDF file
- Microsoft PowerPoint file
- Microsoft Word file
- Microsoft Excel file
- Audio/Video file
- Apple Quicktime file
- RealPlayer file
- Zip Archive file
- Professional Resources
- Browse By Interest
Understanding CDC Travel Health Notices
The U.S. Centers for Disease Control and Prevention (CDC) uses Travel Health Notices (THN) to “inform travelers and clinicians about current health issues that impact travelers’ health, like disease outbreaks, special events or gatherings, and natural disasters, in destinations around the world.”
On April 13, 2022 the CDC announced significant changes to the Travel Health Notices (THN) specific to COVID-19. The structure of the 4 level system will reserve the highest level-'Level 4: Do Not Travel' for only special circumstances such as a healthcare infrastructure collapse or extreme spikes in case counts of COVID-19 levels. This change resulted in 89 countries being removed from the "Level 4: Do Not Travel" list.
CDC Travel Health Notices for Levels 1, 2, and 3 will continue to be based on a 28-day incidence or case counts.
The 4 COVID-19 Travel Health Notice levels are:
Level 4 – Special Circumstances/Do Not Travel
Level 3 – High Level of COVID-19
Level 2 – Moderate Level of COVID-19
Level 1 - Low Level of COVID-19
Level Unknown: Unknown Level of COVID-19
Read more from the CDC on how COVID-19 Travel Health Notices are determined here .
The CDC's standard (non-COVID-19) Travel Health Notice system has 3 levels:
Warning Level 3 – Avoid all non-essential travel
Alert Level 2 – Practice Enhanced Precautions
Watch Level 1 – Practice Usual Precautions
This standard THN system will remain in use alongside the C OVID-19 specific travel health notices introduced by the CDC in 2020.
COVID-19 vaccines currently appear as recommended vaccines on CDC Country Information pages . When COVID-19 vaccines were authorized under an Emergency Use Authorization process, they were not listed on Country Imformation pages by the CDC. Now that the COVID vaccines are authorized under general use guidelines per the FDA, they have been added to a list of recommended vaccines on CDC Country pages.
Colleges, universities, and provider organizations consider CDC Travelers Health Notices and other information provided by the CDC (e.g., vaccinations and immunizations) in their evaluation of the relative health and safety of an education abroad location.
Visit CDC Travelers Health COVID-19 Homepage
Some other sources are:
- WHO Efficiency of Care
- Global Health Security Index assessment
- Harvard Metrics on Case Rates
- WHO current COVID infection rates/spread
- Our World in Data Daily Positive Test Rates
- European Centre for Disease Prevention and Control 14-day cumulative number of COVID-19 cases per 100 000
- CIEE Health Risk Index
- ISOS (COVID-19) Impact Rating
NAFSA Education Abroad Health and Safety
Crisis Management for Education Abroad
Outbound Immigration and Logistical Considerations for Education Abroad During the COVID-19 Pandemic
Government Connection: Understanding CDC Travel Health Notices
clock This article was published more than 2 years ago
CDC travel warning flags 5 Caribbean destinations as ‘very high’ risk for covid
Jamaica and the Dominican Republic are among 15 additions to the agency’s Level 4 list

Federal health authorities on Monday warned against travel to 15 countries and territories, including Costa Rica, the United Arab Emirates and five Caribbean destinations, because of “very high” risk levels of coronavirus .
By issuing Level 4 advisories, the Centers for Disease Control and Prevention said that “even fully vaccinated travelers may be at risk for getting and spreading COVID-19 variants” in those locales. The new additions expand a list of more than 100 destinations to receive the agency’s highest travel warning.
In the Caribbean, the CDC urged people to “avoid travel” to Jamaica, Saint Barthelemy, the Dominican Republic and two island territories of France: Guadeloupe and Saint Martin. The agency also issued its highest coronavirus warning for Peru, Colombia, Fiji, Kuwait, Mongolia, Niger, Romania and Tunisia.
Monday’s alerts deal with some of the most popular beach destinations for Americans. According to federal travel data , more than 4.6 million U.S. citizens traveled to the Caribbean from January through September last year. That exceeds the number of U.S. visitors to any other overseas region, including all of Europe.
Other Caribbean tourist spots designated as highest-risk include the Bahamas, Barbados and Sint Maarten , which is part of the Netherlands and on the same island as Saint Martin.
The CDC’s latest advisories come as some countries ease travel restrictions and project optimism that cases of the highly transmissible omicron variant have peaked within their borders. British officials said Monday that starting Feb. 11, fully vaccinated travelers will no longer have to take a coronavirus test within two days of entering England. Thailand plans to significantly shorten quarantine periods for visitors who are fully vaccinated based on their test results.
Britain to remove testing requirement for fully vaccinated travelers
But the explosion of cases driven by omicron continues to weigh on travel plans, and the CDC has issued a steady stream of warnings.
The CDC is not advising against all travel to Mexico, which saw the most U.S. tourism in the first nine months of 2021, with nearly 20 million American visitors. But it says unvaccinated people “should avoid nonessential travel” there.
The CDC uses a four-level system of coronavirus travel warnings. Destinations are generally moved to the highest tier if they sustain infection levels of more than 500 new cases per 100,000 people over 28 days, though authorities also take testing and the trajectory of new cases into account as well.
The CDC said if people must travel to the destinations that were just marked Level 4, they should get fully vaccinated against the coronavirus first. The agency urges against international trips for those who are not vaccinated, but it says people should get tested one to three days before leaving if they do travel.
Health officials have emphasized that some vaccinated people will contract the virus, particularly as omicron proves more resistant to existing vaccinations. Research shows that omicron tends to cause less severe illness than the delta variant, which became dominant last year.
Vaccinations appear to protect against the most serious infections, experts say, especially for those who have gotten a booster shot.
CDC advises against traveling to Canada, citing coronavirus levels
Traveling to Europe? What to know about 5 countries during omicron.
How to use Biden’s free coronavirus tests on your next trip

- Caribbean News
- Diaspora News
- South Florida News
- Entertainment
The Centers for Disease Control and Prevention (CDC) has issued a Level 2 Travel health notice for individuals travelling to Cuba due to an outbreak of the Oropouche virus.
A Level 2 Travel health notice means travelers should practice enhanced precautions for this destination.
According to the travel notice issued on August 16, multiple cases of Oropouche have recently been reported in US and European travelers returning from travel to Cuba indicating there is ongoing risk.
Oropouche is spread by the bite of infected midges (small flies) and mosquitoes. The CDC advises all travelers to take steps to prevent bug bites during travel, to protect themselves from infection. It says pregnant people should reconsider non-essential travel to Cuba.
Symptoms of Oropouche include headache, fever, muscle aches, stiff joints, nausea, vomiting, chills, or sensitivity to light. Severe cases may result in neuroinvasive disease such as meningitis. Symptoms typically start 3–10 days after being bitten and last 3–6 days. Most people recover without long-term effects. There is no specific treatment for Oropouche.
The CDC says travelers who develop high fever, headache, muscle aches, stiff joints, nausea, vomiting, chills, or sensitivity to light during or within 2 weeks after travel should:
- Seek medical care immediately and tell their healthcare provider when and where they traveled. Learn how to seek medical care during travel.
- Not take aspirin or other NSAIDS (e.g., ibuprofen) to reduce the risk of bleeding.
- Continue to prevent bug bites during the first week of illness to avoid further spread in areas where mosquitoes or biting midges are active.
The CDC currently has a Level 1 Travel health notice for Oropouche virus for parts of Bolivia, Brazil, Colombia and Peru, which reported cases, although the case numbers are declining.
More Stories
Svg pm dr ralph gonsalves conferred japan’s grand cordon of the order of the rising sun, caricom chair calls for increased vigilance amid mpox outbreak, jamaica’s finance minister nigel clarke to leave gov’t for top imf position, haiti faces escalating humanitarian crisis amid underfunding and violence, vaz says no oil discovery in jamaica, montserrat sets nomination day for october 10, st. vincent’s bequia airport reopens 8 weeks after the passing of hurricane beryl, montserrat to hold general election in october, barbados denies case of mpox, dominican republic authorities seize 3,000 pounds of cocaine en route to germany, latest articles, sean kingston and mother appear in broward court for fraud charges, grace atlanta caribbean jerk festival returns on sept. 1, prime minister gonsalves addresses vybz kartel’s visit to st. vincent.


COMMENTS
CDC uses Travel Health Notices (THNs) to inform travelers about global health risks during outbreaks, special events or gatherings, and natural disasters, and to provide advice about protective actions travelers can take to prevent infection or adverse health effects. A THN can be posted for: 1) a disease outbreak (higher number of expected ...
More. Learn about CDC's Traveler Genomic Surveillance Program that detects new COVID-19 variants entering the country. Sign up to get travel notices, clinical updates, & healthy travel tips. CDC Travelers' Health Branch provides updated travel information, notices, and vaccine requirements to inform international travelers and provide ...
Destinations. Measles cases are increasing globally, including in the United States. The majority of measles cases imported into the United States occur in unvaccinated U.S. residents who become infected during international travel. A list of countries with confirmed measles outbreaks can be found on the Global Measles Travel Health Notice (THN).
International Travel Health Notices. Outbreak Resources. ... See previous foodborne outbreak alerts since 2006. June 20, 2024. Outbreak Investigation Resources. Active Investigations of Multistate Foodborne Outbreaks. View foodborne outbreaks CDC is investigating each week. ... CDC helps countries respond to disease outbreaks and stop them at ...
State Department Travel Advisory Updates. In order to provide U.S. travelers detailed and actionable information to make informed travel decisions, the Department of State regularly assesses and updates our Travel Advisories, based primarily on the U.S. Centers for Disease Control and Prevention (CDC) Travel Health Notices (THNs) and secondary factors such as commercial flight availability ...
Coronavirus disease 2019 (COVID-19) is a respiratory illness caused by the virus SARS-CoV-2. The virus spreads mainly from person to person through respiratory droplets and small particles produced when an infected person coughs, sneezes, or talks. The virus spreads easily in crowded or poorly ventilated indoor settings.
Dengue is a year-round risk in many parts of the world, with outbreaks commonly occurring every 2-5 years. Travelers to risk areas should prevent mosquito bites. Country List : Brazil, Burkina Faso, Colombia, Costa Rica, Ecuador, including the Galápagos Islands, French Guiana (France), Guatemala, Guyana, Honduras, Laos, Mali, Mauritius, Mexico, Panama, Samoa, Singapore, Sri Lanka, Sudan ...
All eligible travelers should be up to date with their COVID-19 vaccines. Please see Your COVID-19 Vaccination for more information. COVID-19 vaccine. Hepatitis A. Recommended for unvaccinated travelers one year old or older going to Puerto Rico. Infants 6 to 11 months old should also be vaccinated against Hepatitis A.
CDC uses Travel Health Notices to alert travelers and other audiences to health threats around the world and advise on how to protect themselves before, during, and after travel. With this new configuration, travelers will have a more actionable alert for when they should not travel to a certain destination (Level 4), regardless of vaccination ...
Audience: Clinical Laboratory Professionals Level: Laboratory Advisory On August 16, 2024, the U.S. Centers for Disease Control and Prevention (CDC) issued a Health Alert Network (HAN) Health Advisory about an increase in Oropouche virus disease in the Americas region. Oropouche virus is spread to people primarily by the bite of infected midges and some mosquitoes.
Summary The Centers for Disease Control and Prevention (CDC) is issuing this Health Alert Network (HAN) Health Advisory to notify clinicians and public health authorities of an increase in Oropouche virus disease in the Americas region, originating from endemic areas in the Amazon basin and new areas in South America and the Caribbean.
Level 1: Exercise Normal Precautions. July 26, 2023. Ghana Travel Advisory. Level 2: Exercise Increased Caution. November 20, 2023. Democratic Republic of the Congo Travel Advisory. Level 3: Reconsider Travel. July 9, 2024. Republic of the Congo Travel Advisory.
What to Know About the C.D.C. Guidelines on Vaccinated Travel. In updated recommendations, the federal health agency said both domestic and international travel was low risk for fully vaccinated ...
COVID-19. COVID-19 (coronavirus disease 2019) is a disease caused by a virus named SARS-CoV-2. It can be very contagious and spreads quickly.
CDC uses Travel Health Notices (THNs) to alert travelers and other audiences to health threats around the world and advise on how to protect themselves. On November 21, 2020, CDC adapted its 3-level notice system to a 4-level system for COVID-19 and updated criteria used to determine THN levels. The system was updated to align with the same ...
The CDC recommends avoiding travel to countries at level 4, the highest threat level, which have more than 500 cases per 100,000 residents in the last 28 days. Other level 4 countries include ...
The CDC's own travel health notices also use a four-tier warning system. For many countries newly added to the State Department's Level 4 list, the CDC cites "a very high level of COVID-19."
The CDC maintains an evolving list of travel notices from Level 1 ("low") to Level 4 ("very high"). Last week the agency added 16 destinations to its "very high" risk category ...
The United Kingdom was at Level 3 ("high" risk) on April 18, 2022. (Wayne H/Adobe Stock) CNN's Tierney Sneed contributed to this report. The CDC unveiled its new system for travel risk ...
If your travel plans in Uganda include outdoor activities, take these steps to stay safe and healthy during your trip. Stay alert to changing weather conditions and adjust your plans if conditions become unsafe. Prepare for activities by wearing the right clothes and packing protective items, such as bug spray, sunscreen, and a basic first aid kit.
CDC uses Travel Health Notices (THNs) to alert travelers and other audiences to health threats around the world and advise on how to protect themselves. On November 21, 2020, CDC adapted its 3-level notice system to a 4-level l l system for COVID-19 and updated criteria used to determine THN levels. The system was updated to align with the same ...
What is the CDC Travel Health Notice System? The CDC's standard (non-COVID-19) has 3 levels: Warning Level 3 - Avoid all non-essential travel. Alert Level 2 - Practice Enhanced Precautions. Watch Level 1 - Practice Usual Precautions. This standard THN system will remain in use alongside the C introduced by the CDC in 2020.
The CDC uses a four-level system of coronavirus travel warnings. Destinations are generally moved to the highest tier if they sustain infection levels of more than 500 new cases per 100,000 people ...
The Centers for Disease Control and Prevention (CDC) has issued a Level 2 Travel health notice for individuals travelling to Cuba due to an outbreak of the Oropouche virus. A Level 2 Travel health notice means travelers should practice enhanced precautions for this destination.
The US Centers for Disease Control and Prevention moved five Caribbean island destinations into its highest-risk travel category for Covid-19 on Monday. In total, the CDC moved 15 places to Level ...
Earlier this month, the CDC issued a health alert to notify clinicians and public health authorities of an increase in the disease in the Americas region that has caused two deaths so far this year.
Earlier this month, the CDC issued a health alert to notify clinicians and public health authorities of an increase in the disease in the Americas region that has caused two deaths so far this year.
The Pan American Health Organization issued an epidemiological alert due to the virus spreading in South America and Cuba. ... Sun & Moon. Travel. Climate. Now Playing. What You Need To Know About ...