- Find your local Age UK

- Site search Search term
- Back Information and advice
- Back Money & legal
- Back Benefits and Entitlements
- Attendance Allowance
- Benefit rates 2024-25
- Benefits Calculator – what are you entitled to?
- Bereavement Support Payment
- Carer's Allowance
- Benefits for mixed age couples
- Changes to the benefits system
- Cold Weather Payment
- Council Tax Reduction
- Disability Living Allowance
- Employment and Support Allowance
- Free bus pass and transport concessions
- Free prescriptions for over 60s
- Housing Benefit
- How to apply for a Blue Badge
- How to challenge a benefits decision through mandatory reconsideration
- How to get help with urgent or one-off expenses
- How your benefits are means tested
- Income Support
- Jobseeker's Allowance
- Pension Credit
- Personal Independence Payment
- Returning to the UK after living abroad
- Support for Mortgage Interest
- TV licence concessions
- Universal Credit
- Warm Home Discount
- Winter Fuel Payment
- More money in your pocket information guide
- Back Debt and savings
- Debt help and advice
- Energy advice for the home
- Financial jargon buster: financial terms explained
- How to reduce your water bills
- How to trace old bank accounts & lost money
- Back Income and tax
- What is equity release and how does it work?
- Ways to reduce Council Tax
- How does income tax work?
- How does Inheritance Tax work?
- How to boost your income in retirement
- Equity release information guide
- Back End of life issues
- Back Legal issues
- Finding legal advice
- How to be an executor information guide
- Making a will
- Power of attorney
- Power of attorney information guide
- Thinking about end of life information guide
- What is a living will (advance decision)?
- What is an executor?
- What to do when someone dies
- Wills and estate planning information guide
- What is probate?
- Back Pensions advice
- Annuities explained
- Finding old pensions
- Pension calculator
- Pensions scams and fraud
- State Pension
- What are workplace pensions?
- What pension options do I have?
- Back Scams and fraud
- How to spot a catfish
- Spotting TV Licence scams
- Doorstep scams
- Postal scams
- Phone scams
- What to do if you're the victim of a scam
- Investment scams and fraud
- Avoiding scams information guide
- Help with the cost of living
- Back Consumer advice
- Are landlines being phased out?
- Back Health & Wellbeing
- Back Conditions and illnesses
- Bladder and bowel problems information guide
- Bowel problems
- Coronavirus
- Depression and anxiety
- Hearing loss
- High blood pressure
- Influenza (flu) prevention
- Malnutrition
- Osteoporosis
- Seasonal affective disorder (SAD)
- Urinary incontinence
- Urinary tract infections (UTIs)
- Back Health services

Dental services for older people
9 health tests that could save your life, getting the most from your medicines, getting help when feeling unwell.
- NHS continuing healthcare
Your hospital stay
Gp services for older people.
- Leaving hospital
- Complaining about NHS services and hospitals
What standards you should expect from NHS services
- Your hospital stay information guide
- Back Being active
- Getting active when you find exercise difficult
- Getting active but not sure where to start
- Helping someone to get active
- Preventing falls
- How to look after your feet
- Walking tips
- Physical activity videos to use at home
- Staying steady information guide
- Back Mind and body
- 10 tips for ageing better
- 5 tips to boost your mood
- Getting a good night's sleep
- Your mind matters
- Mindfulness
- Staying cool in a heatwave
- Staying sharp
- Preventing and treating burns
- Back Loneliness
- A Life Less Lonely
- Caring for someone who's lonely
- Feeling lonely
- Back Looking after your health and money this winter
- Keeping warm and well in winter
- Keep your spirits up
- Managing money in winter
- Winter wrapped up information guide
- Winter illnesses
- Back Relationships and family
- Financial and legal tips before remarrying
- Planning for end of life
- Protection from abuse and neglect
- Dating in later life
- Sex in later life
- How to deal with grief after a bereavement
- How to adjust to living alone
- Top tips for grandparents
- Worried about someone?
- Back Care & support
- Back Finding and arranging social care
- Care needs assessment
- Homecare: how to find the care you need at home
- Back Paying for care
- Financial assessment explained
- Paying for residential care
- Paying for homecare
- How much does care cost?
- Back Help & advice for carers
- What is a carer's assessment?
- Financial support for carers
- Balancing working and caring responsibilities
- Caring for someone with dementia
- Looking after yourself as a carer
- What is respite care?
- What to do when your caring role changes or ends
- Carer's checklist
- Back Housing options in later life
- Assisted living and extra-care housing
- Safety in the home
- How to make your home safer and more comfortable
- Specialist housing options
- Renting and social housing
- Homelessness
- Moving in with children and family
- Park homes (mobile homes)
- Sheltered housing
- Back Problems with care
- How to complain about care to your local council
- Problems with homecare
- Back Work & learning
- Back Making the most of the internet
- Computer training courses
- Glossary of online terms
- Getting started on the internet
- Staying safe online
- Keeping in touch using a video call
- Making your device easier to use
- How to download apps
- Email essentials
- What's WhatsApp?
- Using social media
- Is online banking safe?
- How to transfer money and make payments
- Shopping safely online
- Online password security
- Age UK's digital instruction guides
- Back Discrimination and rights
- Changes to immigration status – what is an eVisa?
- EU citizens and settled status after Brexit
- Help for Ukrainian nationals in the UK
- Human rights
- The Equality Act
- Windrush Compensation Scheme information guide
- Windrush Scheme
- Your rights at work
- Back Education and training
- Build up your skills
- Classes and courses
- Higher education and university
- u3a – Later life learning
- Back Looking for work
- Be your own boss
- CVs and job applications
- Job interview tips
- Back Retirement
- Preparing emotionally for retirement
- Paul Lewis: Retirement planning advice
- Living abroad after retirement
- Retirement age
- Back For professionals
- Benefits hub for professionals
- Mental health hub for professionals
- Winter hub for professionals
- Information guides and factsheets
Age UK Advice Line 0800 678 1602
Free to call 8am – 7pm 365 days a year Find out more
Telephone friendship
Get a free weekly friendship call. We'll match you with one of our volunteers. Our service is flexible to suit the different needs of everyone who takes part.
- Sign up for telephone befriending
- Find services near you
- Find charity shops near you
Popular services
- Age UK Advice Line
- Befriending services
- The Silver Line Helpline
- Day Centres
- Exercise and physical activity
- Handyperson services
- IT Training
- Social activities
- Back Services
- Back Get involved
- Back Donate
- Make a donation
- Back Leave a legacy donation in your will
- How to leave a gift in your will
- Get your free gifts in wills guide
- Request your free will writing guide
- Making and amending your will to include a gift to Age UK
- Information for executors
- The difference a gift in your will could make
- Ways to write your will
- Free Wills Month 2024
- Will Aid November 2024
- Back Donate to our shops
- Sustainability
- Shop online
- Back Donate in memory
- Make a donation in memory
- Fundraise for Age UK in memory of your loved one
- Make a one-off donation
- Funeral donations and collections
- Set up a Tribute Fund
- Meaningful ways to remember your loved one
- Make a major gift
- The difference your money makes
- Our professional fundraisers
- Back Fundraise
- Back The innocent Big Knit – get knitting for Age UK
- innocent Big Knit updates
- Run for charity
- Back Fundraising ideas
- Most popular ideas
- Sporty ideas
- Fundraise at work
- Fundraise at school
- Fundraise while you celebrate
- Fundraise as a community
- A-Z of fundraising ideas
- Get your free fundraising guide
- Pay in your fundraising
- Fundraising resources
- Leeds Abbey Dash
- Back Stream for Ages
- Your free downloads
- Back Lottery and raffle
- Play the Age UK lottery
- Tuesday Treat Draw
- Play the Age UK raffle
- Gift the Lottery
- Player Zone
- How every entry helps
- Are you a winner?
- Lottery and Raffle rules
- Back Volunteering
- Telephone Friendship Service volunteering
- The Silver Line Helpline volunteering
- Connect and Support Service volunteering
- Age UK shops volunteering
- Local Age UK volunteering
- Support our campaigns
- Back Corporate partnerships
- Why partner with Age UK
- Back Ways we could work together
- Can your company support the Age UK Telephone Friendship Service?
- Help Age UK become Morrisons’ next charity partner
- Latest jobs with Age UK
Age UK. Know what to do.
Last year, over 10 million people trusted us to help them with some of the biggest issues in their lives. Learn more about how we help.
How your support helps
Here's how, with your support, Age UK is supporting older people through the cost of living crisis.
- See the difference your donations make
Making older people's voices heard
- Age UK know what to do
- Campaigning with older people
- Discover - news, stories and features
- Media Centre
- Policy and research
- Wellbeing programmes
- Politics and government
- Back Our impact
- Back Buy products
- Back Over-50s Insurance
- Car insurance
- Home insurance
- Motor breakdown cover
- Travel insurance
- Travel insurance with medical conditions
- Back Independent living
- Bathing Solutions
- Stairlifts and Homelifts
- Personal Alarms
- Back Financial services
- Funeral Plans
- Legal services
- Back Healthcare
- Incontinence products
Health services
Although your GP doesn’t need to be your first point of contact if you're feeling unwell, everyone should be registered with a GP. If you're not, you should register with a practice as soon as possible, even if you don't currently have any health problems.
What does a GP do?
What services should i look for in a gp surgery, how do i register with a gp surgery, what if i'm too ill to visit my gp, what if i'm not registered with a gp or i'm away from home, what support can i get if i have a long-term condition.
Your General Practitioner (GP) can give you medical advice, treatment and prescribe medication.
Your GP can also refer you to other healthcare professionals to diagnose or treat specific aspects of your condition. For example, they may refer you to a chiropodist, for a hearing test, or to your local falls prevention service. These other health professionals may visit you at home or hold clinics at a local practice, health centre or hospital.
Your GP practice must allocate everyone a named, accountable GP. This GP will oversee your care and take responsibility for evaluating your current physical and psychological needs. Though this doesn’t mean the named GP is the only doctor at your practice who will or can provide care.
If you're joining a new surgery, ask about the availability of services that may be important to you, such as:
- how the appointment system works
- how far in advance you can book a non-urgent appointment
- extended opening hours
- support for carers
- availability of male and female GPs and nurses
- wheelchair access
- staff who speak languages other than English.
Some surgeries offer a 24-hour online service, which you can use to book appointments with a GP of your choice, cancel appointments, order repeat prescriptions and view your summary care record. Speak to the receptionist to find out what online services your GP surgery offers and how to register for online access.
If you have difficulty finding a practice with space for new patients, contact NHS England – it's their responsibility to find a GP practice for you.
Find out more about online services on the NHS website
You can register with a GP surgery over the phone, online or in person.
You don't need proof of ID to register with a GP, but you may find it helpful to have your passport or birth certificate handy while you're filling in your details.
Find out more about registering with a GP on the NHS website
If you can't visit your GP surgery for medical reasons, you can ask your GP to make a home visit. If possible, try to call your GP in the morning if you think you'll need a visit the same day. Your GP surgery should have accessible information explaining how to request a home visit.
If you need to see your GP but can't make it into the surgery, they must offer a home visit instead. They should factor in how urgent your condition is when arranging a home visit.
Your GP might also be able to give you advice through a telephone or video consultation as an alternative.
You should always be able to see a GP if you need urgent attention. If you become ill while you're away from home or you haven't registered with a GP, you should contact the nearest surgery and ask them to see you.
If you'll be living away from your usual address for up to 3 months, you can register as a temporary patient at a local practice. You'll still be able to remain registered as a patient with the GP where you normally live.
If you have a long-term condition, your GP should help you understand and manage your own care. This may include drawing up a care plan to help you manage your condition on a day-to-day basis and recognise symptoms that you should report to your GP.
It may also include creating an 'information prescription'. This is a collection of information that your GP thinks is helpful to you at that time and will help you understand your condition, as well as ways to prevent any further complications. This can be done with the help of the NHS website, which helps you find reliable sources of information about your condition.
Want more information?
NHS services factsheet (828 KB)
- Find out more about what you can expect from NHS services
- Visit the NHS website
- Find out how to contact NHS England
We're here to help
We offer support through our free advice line on 0800 678 1602. Lines are open 8am-7pm, 365 days a year. We also have specialist advisers at over 120 local Age UKs.
About the Age UK Advice Line Find your local Age UK
Share this page
- Share on Facebook
Last updated: Apr 08 2024
You might also be interested in...
Find out more about your rights and responsibilities as a patient in the NHS Constitution.
Regardless of age, very few people feel well all the time. Here are some ways you can get help when you're ill.
Find out more about some routine health checks that are quick to perform and can help you spot signs of illness.
Find out more about how to prepare for a hospital stay and what you can do to prepare your home for your return.
Find out how to get the most from your medicines, including how to get the most out of your pharmacy.
Find out more about how to take care of your teeth and gums, and what services are available on the NHS.
Become part of our story
- Please enter a valid email address
Back to top
GP mythbuster 71: Prioritising home visits
It is good practice for GP practices to have systems in place to triage and prioritise home visits.
Since the coronavirus (COVID-19) pandemic, the need for a home visit should be continue to be carefully assessed. The British Medical Association (BMA) and Royal College of General Practitioners have published COVID-19 Workload Prioritisation Unified Guidance which explains response levels. The guidance outlines types of work that should be undertaken in primary care, depending on:
- COVID-19 prevalence
- other workload
- workforce factors
The British Medical Association (BMA) has produced a COVID-19 toolkit for GPs and GP practices .
NHS England issued a patient safety alert to raise awareness of the need to have a system in place to assess:
- whether a home visit is clinically necessary , and
- the urgency of need for medical attention.
The alert states that:
"This can be undertaken, for example, by telephoning the patient or carer in advance to gather information to allow for an informed decision to be made on prioritisation according to clinical need. In some cases, the urgency of need will be so great that it will be inappropriate for the patient to wait for a GP home visit and alternative emergency care arrangements will be necessary."
"Many practices will already have systems in place to manage home visits. Where this is the case, consideration should be given to whether a review is required in light of this alert. The review should also consider whether all clinical and non-clinical staff involved in the process are aware of their responsibilities when managing requests for home visits, and if any outstanding training needs exist.”
GPs should also consider whether alternate ways of assessing the patient are appropriate. For example, video call, telephone calls or the use of virtual wards in care homes.
When delegating home visits, the provider must ensure that the Health Care Professional (HCP) has the necessary:
- competence and
- training to deliver the home visit.
The HCP should also receive appropriate supervision and support from the clinical team. Practices should ensure that the person allocated is competent to carry out home visits.
When we inspect
We will expect to see evidence of how the provider has assured themselves of the capability of non-medical HCPs, to whom they delegate home visits. This should include a process of assurance: both on initial delegation of the role and how the HCP’s capability is maintained on an ongoing basis. It should include audit of:
- their clinical decision-making
- prescribing decisions when relevant and
- a system for escalation to a senior clinician when necessary.
We use these regulations when we review if the practice is safe, effective, responsive, caring and well led. This mythbuster relates to:
- Regulation 9 (Person centred care)
- Regulation 12 (Safe care and treatment)
It is part of our key lines of enquiry (KLOEs). One of our key questions is whether services are organised so that they meet people’s needs. In particular, KLOEs:
- S2 Managing Risk
- S3 Safe care and treatment
- E3 Staff skills and knowledge
- E4 How staff, teams and services work together
- R1 Person centred care
- R3 Timely access to care and treatment
- WL8 Learning, improvement and innovation .
We may look at how the practice:
- manages and prioritises home visits
- recognises a deteriorating patient
- works with other professionals
- manages care planning, referrals and investigations.
We may also look at:
- the practice’s processes and systems to monitor patient safety through reporting patient safety incidents
- how they learn from these incidents and significant events.
This patient safety alert shows how important it is for GP practice staff to report all patient safety incidents to the National Reporting and Learning System (NRLS). Lessons can be learned across general practice.
Further information
- GP mythbuster 24: Reporting patient safety incidents to the National Reporting and Learning System (NRLS) for GP practices
- GP mythbuster 66: Advanced nurse practitioners and primary care
- GP mythbuster 100: Online and video consultations and receiving, storing and handling intimate images
- GP mythbuster 102: Pulse oximetry and monitoring vital signs outside the GP practice
- Patient Safety eForm (nrls.nhs.uk)
GP mythbusters
Snippet gp mythbusters rh.
Clearing up some common myths about our inspections of GP and out-of-hours services and sharing agreed guidance to best practice.
See all issues:
- GP mythbusters: listed by key question
- GP mythbusters: full list
- GP mythbusters: recently updated
For more information on the RSV Vaccination please click here
Arrange a GP home visit
If you or someone in your family is unable to come to the surgery because of illness, then you can arrange a home visit.
You can arrange a visit by using our online form and explaining your problem. We can then arrange to see the most urgent cases first.
If you are able to come to the surgery, then we would appreciate it if you could book an appointment. This is because home visits can take up to six times longer than an in-person surgery visit, so it helps the GP to see more patients if you can try to come to the surgery.
You can also bring your children into the surgery if they have a high temperature.
How to arrange a home visit
You can arrange for a GP or Healthcare Professional to see you by booking a home visit online. You can also be visited at home by a community nurse if you are referred by your GP/Healthcare professional. You should be visited at home by a health visitor if you have recently had a baby or if you are newly registered with a GP and have a child under five years.
Change or cancel a home visit
You can change or cancel a home visit online. If your home visit is no longer convenient for you, then it's important to let us know so that we can help other patients.
Appointments
To book an appointment to see your GP or nurse, you can go to our Appointments page to find out more information.
If you need help when we're closed
If you need medical help when we're closed, then you can call 111 .
- Entertainment
- Royal Family
- Food & Drink
- Women's Health
- Mental Health
- Sex & Relationships
- Documentaries
- Tyla Recommends
To make sure you never miss out on your favourite NEW stories , we're happy to send you some reminders
Click ' OK ' then ' Allow ' to enable notifications

Three key signs you need to see a GP if you snore at night
You might need to visit your gp if you do one of these three little-known signs when you snore.
Charlotte Bend
Sleeping in different positions, elevating your feet, nose tape, different pillows or even ear plugs.
Snorers will know this list all too well, with many couples desperately trying to soothe their ailment to help their partner get some sleep .
But now a list of three key warning signs has been revealed for snorers - or their partners - to take note of.
Regular snorers are not usually subject to any serious condition and it is a very common problem.
But the NHS has a handy list of key signs to look out for that could signal something more concerning, recommending those that spot the symptoms head to their GP to get things checked out.
Knowing what to look out for could make all the difference with these three little-known alerts.
Why do I snore?

Snoring can be caused by any number of things, which is why it can be difficult to know how to treat it.
Often, it is caused by the position of someone's tongue, mouth, throat or airways which causes vibrations as you breathe.
You're more likely to snore if you are:
- someone who drinks too much alcohol
- sleeping on your back
What do the experts say?
Adeel ul-Haq, from bunkbeds.co.uk, has previously suggested one simple trick that's slightly bizarre.
Those who are desperate to soothe their snoring could try the hack which takes less than five minutes a day.
The sleep expert revealed to GloucesterLive that strengthening the muscles in your mouth could be a simple way of fixing your nighttime ailments.
All you have to do is grab a spoon, hold it in one hand and bring it to the front of your mouth.
Then you should push your tongue out, while bringing the spoon back in the opposite direction, being gentle to not hurt yourself.
According to Adeel, holding this position for five to ten minutes and repeating up to five times a day should mean you 'notice an improvement in your sleep quality'.
Three warning signs
Many may have already tried to lose weight or alter their drink and diet habits.
Yet, for some these lifestyle changes will not have made a difference.
According to the NHS website, those who have tried lifestyle changes and have not had any success should see their GP.
The second sign is for those whose snoring has had a 'big impact'.
This doesn't just mean for your partner but also for you.
Finally, if you feel sleepy during the day or your partner notices you stop breathing during your sleep, then you may have sleep apnoea.
Those making gasping or choking noises while they sleep could also have the condition, which can be serious if not treated.
For any of these three key signs, the NHS has recommended that sufferers head to their GP to check that their snoring is not a sign of something more serious.

How to treat snoring?
There are many ways to fix snoring but the best cause of treatment won't be the same for everybody.
Some try wearing devices to bring their tongue forward whilst they sleep.
Others try a chin slap to hold their mouth closed.
It seems a bit of trial and error is needed, with surgery even being an option for those who struggle to find a solution on their own.
Topics: Health , Sleep , NHS
Choose your content:

Why your hair might be getting greasy so quickly and it's not always your shampoo
Your hair could be getting greasy for a number of reasons, but there is a quick fix.

Groom had ‘worst headache of his life’ that ended up being something way more sinister that ‘popped’ on his wedding day
Nathan vaughan had to leave his own wedding early as a result of what he believed to be an intense migraine.

Little-known effects your period may be having on your hair and skin
Your period does a lot more than give you cramps each month.

- Surprising reason why you might wake up with a dry mouth and when to see a GP about it
Waking up in the morning with a dry mouth could mean you've just been snoring, however, there are some reasons you should speak to a GP
- One food that could cure hiccups as advice issued on when to see the GP
- Reason why you have no energy at the minute and what you can do to fight it
- Reason why you could be experiencing TATT and what you can do to help it
- GP practice services
- Health advice
- Health research
- Medical professionals
- Health topics
Advice and clinical information on a wide variety of healthcare topics.
All health topics
Latest features
Allergies, blood & immune system
Bones, joints and muscles
Brain and nerves
Chest and lungs
Children's health
Cosmetic surgery
Digestive health
Ear, nose and throat
General health & lifestyle
Heart health and blood vessels
Kidney & urinary tract
Men's health
Mental health
Oral and dental care
Senior health
Sexual health
Signs and symptoms
Skin, nail and hair health
Travel and vaccinations
Treatment and medication
Women's health
Healthy living
Expert insight and opinion on nutrition, physical and mental health.
Exercise and physical activity
Healthy eating
Healthy relationships
Managing harmful habits
Mental wellbeing
Relaxation and sleep
Managing conditions
From ACE inhibitors for high blood pressure, to steroids for eczema, find out what options are available, how they work and the possible side effects.
Featured conditions
ADHD in children
Crohn's disease
Endometriosis
Fibromyalgia
Gastroenteritis
Irritable bowel syndrome
Polycystic ovary syndrome
Scarlet fever
Tonsillitis
Vaginal thrush
Health conditions A-Z
Medicine information
Information and fact sheets for patients and professionals. Find out side effects, medicine names, dosages and uses.
All medicines A-Z
Allergy medicines
Analgesics and pain medication
Anti-inflammatory medicines
Breathing treatment and respiratory care
Cancer treatment and drugs
Contraceptive medicines
Diabetes medicines
ENT and mouth care
Eye care medicine
Gastrointestinal treatment
Genitourinary medicine
Heart disease treatment and prevention
Hormonal imbalance treatment
Hormone deficiency treatment
Immunosuppressive drugs
Infection treatment medicine
Kidney conditions treatments
Muscle, bone and joint pain treatment
Nausea medicine and vomiting treatment
Nervous system drugs
Reproductive health
Skin conditions treatments
Substance abuse treatment
Vaccines and immunisation
Vitamin and mineral supplements
Tests & investigations
Information and guidance about tests and an easy, fast and accurate symptom checker.
About tests & investigations
Symptom checker
Blood tests
BMI calculator
Pregnancy due date calculator
General signs and symptoms
Patient health questionnaire
Generalised anxiety disorder assessment
Medical professional hub
Information and tools written by clinicians for medical professionals, and training resources provided by FourteenFish.
Content for medical professionals
FourteenFish training
Professional articles
Evidence-based professional reference pages authored by our clinical team for the use of medical professionals.
View all professional articles A-Z
Actinic keratosis
Bronchiolitis
Molluscum contagiosum
Obesity in adults
Osmolality, osmolarity, and fluid homeostasis
Recurrent abdominal pain in children
Medical tools and resources
Clinical tools for medical professional use.
All medical tools and resources
General health and lifestyle
How to choose the right GP for you

Peer reviewed by Dr Sarah Jarvis MBE, FRCGP Last updated by Gillian Harvey Last updated 6 Apr 2021
- Download Download Article PDF has been downloaded
- Share via email
If you've recently moved or have decided to change GPs for another reason, it's important to get registered as soon as possible. Before you make your selection, it's worth taking the time to check out different GP practices to find the one that best meets your needs.
In this article :
Why make a change, why else do people change, finding a practice, what should i look for, special interests and services, how to change gp practice, what if my registration is refused.
There are many things to consider when choosing a GP but taking the time to do some research and consider your options can help you to make the right decision.
Continue reading below
Patients are permitted to change GPs for any reason. It may be something you choose to do because of personal preferences, or after hearing about a specific service offered at a different GP practice. You may also decide to move GPs because the location is more convenient - close to your child's school, or near to your place of work.
Is a change necessary?
It's worth knowing that, even if you move areas, you might be able to stay with your current GP.
As GPs are no longer required to focus on a strict catchment area, they may be willing to accept you as a patient even if you have moved. If this is something you wish to explore, you need to check with the practice whether they are happy with this and you may need to re-register. It's also important to remember that if you are likely to need home visits, this may not be possible if your GP is too far away.
If your move is temporary, it may be better to register as a temporary resident with a local GP, while staying registered with your current GP. You can register as a temporary resident for up to three months.
Patient-doctor relationship
Sometimes a bad experience or a personality clash can cause people to want to change their GP. This may sometimes mean gravitating towards a different doctor within the same practice, but some patients prefer to change GP practice altogether.
"Some people may have just had a bad experience and feel they have lost confidence," explains GP Dr Jeff Foster .
Having a good patient-doctor relationship is an important part of receiving medical care. "At heart a GP is the only medical specialist that looks after a patient as a whole. We care for patients before they are born, through childhood, adulthood, and as they decline and reach the end of their lives. We are often the last doctor to see a patient alive," explains Foster.
"We know our patients, and we are our patients' advocates. This has multiple benefits including the ability of a patient to feel they can open up to us about issues they may never tell anyone else. 90% of all clinical interactions occur in primary care so it is essential patients feel they can open up to us. This can be in the form of disclosing abuse, mental health, personal issues such as erectile dysfunction or just to allay the fears of normal life and to be someone to listen to when no one else will.
"It also means that we know our patients and when something is wrong we can often pick up on the subtle signs that would otherwise be missed."

Can a doctor remove a patient?
As well as patients choosing to switch doctors, sometimes doctors will decide to remove a patient from their list. "When there is deemed to be an irreversible breakdown in the doctor/patient relationship - for example, because a patient is abusive towards staff - the practice may remove a patient from their list. If patients repeat this behaviour amongst all local practices, those patients are forced to attend specific designated 'secure' units for their care," explains Foster.
Patient picks for Healthcare

Clinical trials - helping to keep your medicines safe.
#MedSafetyWeek, promotes the Yellow Card scheme where you can report any suspected side effects from your medicine or health device. But, thanks to all the hard work that goes on before any medicines or devices come to the market, it is not something you will hopefully have to do very often. All new drugs and jabs have to be thoroughly tested before they are allowed to be prescribed, which requires people to take part in clinical trials. Although these trials may sound scary, scientists go to great lengths to ensure they are safe. But how?
by Lydia Smith

Doing regular physical activity can make people feel good about themselves and it can have a number of benefits for health. For example, it reduces the risk of developing heart disease, stroke, high blood pressure, many cancers, type 2 diabetes and 'thinning' of the bones (osteoporosis). Regular physical activity also helps to control weight and ease stress. Ideally, the aim should be at least 30 minutes of moderate-intensity physical activity on at least five days of the week but even 10 minutes is better than nothing. You should aim to do at least a couple of sessions of muscle-strengthening activities per week as well.
by Dr Pippa Vincent, MRCGP
To view the details of practices within a certain postcode, check out the NHS's Services Near You facility, which will list practices within an area. Through this service you will be able to check opening hours, the specific services offered and other important information.
It's also worth talking to family or friends with experience of a certain practice, who may be able to offer advice or recommendations based on personal experience. "People often hear about a good practice in their area and may want to join based on specific doctors who work there," agrees Foster.
Your reasons for choosing a certain GP may be different due to your personal preferences or medical needs. However, it's worth checking the following to find a practice that ticks the right boxes for you.
Personal service
As GP surgeries can be very busy, you will generally register with a practice rather than an individual GP, due to demand. But some practices offer a 'personal doctor' policy where you register with a GP and can only see them if on their list.
This could be worth looking into if forming a close relationship with a personal GP is particularly important for you - for example, if you have ongoing health needs. However, do remember that you may have to wait longer to see a particular GP - if rapid access is your priority, you may prefer a practice which allows you to book with the next doctor available.
Accessibility
Think about how you might travel to the practice. If you rely on public transport, is it close to a bus or train route? If you drive, think about where you might park. If you have specific access needs - for example, if you have limited mobility or are in a wheelchair - you may need to check whether there are dedicated parking spaces, ramps and other facilities.
Opening hours
What are the opening hours offered? Do they suit your usual routine? Some GPs may offer evening or early morning appointments which could be a useful factor for those working full-time.
Online services
When the COVID-19 pandemic started, all practices were required to screen their patients first through telephone, video or online form submission before seeing them face to face. You may prefer a practice which needs you to submit an online form about your symptoms first - you won't need to wait for a receptionist to be available to answer the phone. Or you may prefer to speak to a receptionist.
Many GPs now offer online booking - for example, with Patient Access . In future (pandemic permitting) it may be possible to book face-to-face appointments directly, but currently many practices allow you to book video or telephone appointments online.
Some practices may allow patients to email their GP directly. If you'd be interested in accessing your GP in this way, it's worth checking out what online services your GP offers.
While all GPs are qualified to treat and diagnose a wide variety of illnesses, and make referrals to specialists where necessary, some GPs develop a 'special interest' in a particular area - for example, dermatology, women's health or diabetes. This means that alongside their existing knowledge, they will have accumulated additional expertise about their area of interest.
If you suffer from a particular complaint - for example, a skin issue that may need regular treatment - it's worth checking out whether there's a doctor with a special interest in this area.
In addition, some practices may offer services that others don't. "Some practices may offer additional services such as family planning, coil fitting, or minor ops - this influences a patient's decision," says Foster.
GPs and gender
Some patients may feel more comfortable seeing a doctor of a certain gender. If you are someone who has personal reasons for this, it's worth checking out whether there are doctors of your preferred gender at a practice.
Whilst all GP practices are required to treat patients equally under the Equality Act, if you are LGBTQ+ it may be important to you that your practice has a visibly LGBTQ+ friendly approach, has support groups or has GPs who are especially knowledgeable about issues specific to your community. It's worth speaking to friends, doing some online research and speaking to the practice if you have specific requirements.
Once you have made a decision, you will then need to contact the practice and fill in a registration form with your NHS and personal details, and information about your previous doctor so that medical records can be requested.
Often the registration can be carried out via email or over the phone, but if you can make a visit, it can be useful way to gauge additional information such as whether the practice feels friendly and welcoming. This likely won't be possible during the pandemic as GP practices have restrictions on who can come in, to keep patients and staff safe.
Some GP surgeries may be unable to accept your registration for a number of reasons. If the practice has no capacity or feels your needs would be better met elsewhere - perhaps due to specific services you use or your location - they have the right to refuse your registration. If this happens, the practice should share their reasons with you.
Article history
The information on this page is peer reviewed by qualified clinicians.
6 Apr 2021 | Latest version
Last updated by
Peer reviewed by
6 Apr 2021 | Originally published

Are you protected against flu?
See if you are eligible for a free NHS flu jab today.

Feeling unwell?
Assess your symptoms online for free
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
The PMC website is updating on October 15, 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Br J Gen Pract
- v.70(695); June 2020

GP home visits: essential patient care or disposable relic?
Introduction.
The GP home visit has long been regarded as an integral element of NHS general practice that is needed to support both proactive and reactive care to patients in the community. 1 , 2 There are increasing numbers of people living with multimorbidity and frailty, many of whom have complex healthcare needs and limited levels of social support. Now with the new challenges around providing care at home due to the COVID-19 pandemic, it could be argued that home visits or virtual consultations with patients in their homes are set to become a more essential element of general practice, including in the provision of acute care out of hours. Consulting with patients in their homes provides unique opportunities to develop insights into how illness affects their lives. However, with workloads in NHS primary care rising, and increasing pressures on the GP workforce, the place of home visits in core general practice provision is facing increasing challenge.
GPs DEBATE HOME VISITING
The requirements of the current GP General Medical Services (GMS) contract in relation to home visiting are broad. 3 The contract is not prescriptive about who should visit or where the visit should take place, and states that the decision to visit is dependent on the opinion and agreement of the GP contractor. In November 2019, the Local Medical Committee (LMC) conference debated the current contractual requirements and a motion was narrowly passed to instruct the General Practitioners Committee (GPC) (the negotiating arm of the British Medical Association) to ‘remove the anachronism of home visits from core contract work’ . 4 The majority backed a motion to negotiate a separate acute service for urgent visits.
Reporting of the LMC debate in the national press and social media highlighted how emotive the issue of home visits is, and the diversity of views among GPs that exist around their value. They were described by some as a service that is regarded by patients as an entitlement, available for purposes of convenience. 4 It is likely that GPs working in practices that are short-staffed and overwhelmed by workload pressures are more likely to view home visits as an inefficient use of their scarce resources. Others considered home visits a vital component of general practice, arguing that when patients are unwell at home it is generalist doctors who are best placed to assess them. There were concerns that removing home visits from the GP contract would compromise the values of general practice, sending a message to patients that their doctor no longer cares for those who may have pressing clinical needs but wish to be treated at home.
WHAT DO WE KNOW ABOUT GP HOME VISITING?
In a healthcare system where it is expected that contracts are informed by robust evidence-based medicine, the lack of evidence regarding GP home visits, including out of hours, is striking. There has been relatively little research to understand the circumstances in which patients request GP home visits, when and why GPs undertake home visits, and how outcomes can be optimised within a resource-constrained health service. What is known is that over the last 50 years there has been a steady decline in the extent to which GPs visit patients in their homes in the UK and internationally, 2 , 5 , 6 and that not all GPs are convinced of their benefits. 1
Some GP consultations with patients at home are reactive when there is an acute and sudden deterioration in their health, including out of hours. The visiting professional must skilfully balance the risks of continuing care at home against admission to hospital. Others are more proactive, to monitor and plan care for those with long-term health conditions that may prevent them from attending the surgery. Research suggests that GPs do not tend to dispute visit requests for vulnerable, older people. 1 For patients who are dying, there is a positive association between GP home visit rates and achieving home as the preferred place for end-of-life care. 7 GPs who gain experience of home visiting during their training are more likely to undertake home visits post-qualification. 8 GP visits to residential and nursing care homes, and the quality of care delivered, have been described as particular areas of concern. 9 Little is known about responses to other patient groups who may benefit, including: those with mental health concerns; physical disabilities; complex care needs; or those who are unwell with potentially infectious diseases, such as children who may be advised not to attend the GP surgery. Patients appreciate home visits and feel that their relationship with their GP improves as a result. 10
Although GP consultations in patients’ homes are likely to require different consultation skills from those that apply within the surgery setting, the requirements for training in the conduct of GP home visits are ill defined and are largely left for the trainee and their trainer to negotiate. For many trainees, there may be limited opportunity for their home visits to be observed, because of logistical and time constraints. 11 Formative assessment tools (Clinical Observational Tools) for home visits are lacking, and summative assessment of a simulated home visit (within the MRCGP Clinical Skills Assessment) occurs in only half of exams.
Many types of home visit have already been subsumed by other services, such as specialist community teams, early visiting services, and care home teams. Although this can be seen as relieving pressure on overstretched general practice, an unintended consequence is the fragmentation of care associated with multiple specialist teams providing care in the patient’s home. It also calls into question the role of general practice in the management of such complex patients. Obtaining timely information, communicating with each visiting specialist team, and overseeing such care risks adding to the GP workload. 12 As Abrams et al highlight in their realist review of delegated home visiting services in this issue, there is more to be done to understand how such services can be implemented effectively. 13 Research is needed to inform delegation processes, and effective system implementation is needed to support such services and to understand the impact on patient satisfaction, long-term health outcomes, and cost. 13 A pertinent issue is the need for clarity around roles and responsibilities, so that the professional status and autonomy of all involved are understood and valued. This is most likely when trusted professional relationships are developed over time and where the facility to share information effectively exists. 13
‘Good general practice will always consist of patients feeling at home with their doctor and of doctors feeling at home with their patients.’ 12 In the context of burgeoning demand and underfunding of workforce and resources, there is a need to listen to the diversity of views among GPs and primary care colleagues concerning the future of home visits. Robust research is needed to provide understanding into the value of GP consultations in patients’ homes, both through visiting and using telemedicine, and how best to optimise the delivery of primary medical care, particularly for housebound patients, 24 hours a day, 7 days a week. Increased understanding into the nuances and impact of GP home visits on patient care and the wider healthcare system would form an important evidence base to inform NHS policy and the training and development of the primary care workforce, and is necessary before changes are made to the GP core contract.
Freely submitted; externally peer reviewed.
After 37 years of pioneering health journalism, community engagement, and empowerment through information, we have now ceased operations.
This website will be accessible until September 2025, with all the information being up to date as of July 2024.
If you are a supplier, or another partner you can contact our legacy email address as [email protected] with any queries.
We extend our heartfelt thanks to everyone who supported our vision for a world where HIV is no longer a threat to health or happiness. Together we have made a difference.
With Gift Aid, your generous donation of £ 10 would be worth £ 12.50 at no extra cost to you.
I am a UK taxpayer and I understand that if I pay less Income and /or Capital Gains Tax than the amount of Gift Aid claimed on all my donations in the relevant tax year, it is my responsibility to pay any difference.
In our 35th year we’re asking people to donate £35 – that’s just £1 for every year we’ve been providing life-changing information. Any donation you make helps us continue our work towards a world where HIV is no longer a threat to health or happiness.
- £5 allows us to reach millions of people globally with accurate and reliable resources about HIV prevention and treatment.
- £10 helps us produce news and bulletins on the latest developments in HIV for healthcare staff around the world.
- £35 means we can empower more people living with HIV to challenge stigma with our information workshops, videos and broadcasts.
Where to get HIV treatment

- In the UK, HIV treatment is provided at specialist clinics within the NHS.
- HIV medications are dispensed at hospital pharmacies or may be provided by home delivery.
- HIV treatment is provided free of charge, regardless of immigration status.
This information is aimed at people who are using the UK National Health Service (NHS), but it may be helpful even if you live elsewhere.
Most people living with HIV in the UK attend specialist HIV clinics or sexual health clinics, which can be found in most areas of the country. Most HIV clinics are ‘open access’. This means that you don’t need a referral from your GP (family doctor) or anyone else to use one. You can simply phone up and ask to register as a patient. You choose which HIV clinic to use.
GPs are not able to prescribe antiretroviral drugs.
You will get a prescription for your HIV treatment at your HIV clinic. Take this to either the specialist HIV pharmacy (in larger clinics) or to the hospital’s outpatient pharmacy. A high-street chemist will not dispense anti-HIV medications, unless your clinic has an agreement with a community pharmacy.
You should be given supplies to last until your next clinic appointment. Once you are stable on HIV treatment, with an undetectable viral load, your clinic will often suggest you receive your anti-HIV drugs by delivery to a place of your choice, or by collection from a community pharmacy. However you will still need to attend regular HIV clinic appointments to have your health monitored.
Always make sure you have enough medication to last until your next clinic appointment, as well as a small supply of spares, at home. If you think you might run out before this, contact your clinic as soon as possible to arrange a further supply until your next appointment.
The pharmacist will ask you if you are allergic to any medicines and explain how to take the drugs that have been prescribed to you. Pharmacists can help you with managing your medication use, including adherence , side-effects , drug interactions, food and drink requirements , storage, pill swallowing, and advice on taking your medicines while travelling .
In England, all HIV care and the anti-HIV medications provided through NHS HIV clinics and sexual health clinics are free (including no prescription charge), whatever someone’s immigration status is. In Scotland, Wales and Northern Ireland, people are not normally charged for HIV treatment and care, although the law still says they can be if they are of uncertain immigration status.
There's more information about access to the NHS for migrants on another page. An HIV support organisation can help you if you are concerned about being charged for treatment.
You can use our HIV services finder to locate HIV clinics near you.
Cookies on GOV.UK
We use some essential cookies to make this website work.
We’d like to set additional cookies to understand how you use GOV.UK, remember your settings and improve government services.
We also use cookies set by other sites to help us deliver content from their services.
You have accepted additional cookies. You can change your cookie settings at any time.
You have rejected additional cookies. You can change your cookie settings at any time.
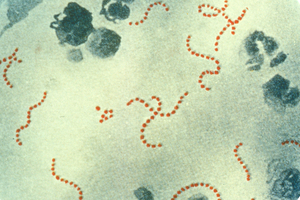
UKHSA update on scarlet fever and invasive group A strep
Latest data from the UK Health Security Agency (UKHSA) on scarlet fever and invasive group A streptococcus cases.
Latest update
The latest data from the UK Health Security Agency ( UKHSA ) shows that scarlet fever notifications are stable and in line with what we would generally expect to see at this time of year.
So far this season (from 12 September 2022 to 7 May 2023), there have been 55,872 notifications of scarlet fever, compared to 54,394 in the last update on 20 April. In the last comparable high season (from September 2017 to September 2018), there were 30,768 scarlet fever notifications overall across the year.
While invasive group A streptococcus ( iGAS ) is still a very rare infection, notifications are slightly higher than we would expect at this time of year and remain relatively high in children compared to what we typically see. As in previous seasons, the majority of iGAS cases have continued to be among those aged over 45 years, particularly in those aged over 75 years.
So far this season, there have been:
- 3,287 iGAS cases across all age groups, up from 2,965 in the last update on 20 April – this is compared to 2,898 across the whole of the last comparably high season in 2017 to 2018
- 761 iGAS cases in children aged 18 years and under, compared to 701 in the last update – this is compared to 205 cases in the 2017 to 2018 season
Sadly, so far this season, there have been 426 deaths (from any cause recorded within 7 days of an iGAS infection diagnosis) across all age groups in England, compared to 401 in the last update. This figure includes 48 children aged under 18 years in England, an increase of one since the last update. In the September 2017 to September 2018 season, there were 354 deaths in total across the season, including 27 deaths among children aged under 18 years.
Dr Colin Brown, Incident Director at UKHSA , said:
While scarlet fever notifications are in line with what we typically see at this time of year, we are still seeing relatively high levels of invasive group A strep infections in the oldest and youngest age groups. It is important that we continue to help stop the spread of all germs in the community and to vulnerable groups. Wash your hands regularly and thoroughly, catch coughs and sneezes in a tissue, and keep your home well ventilated. If you are unwell with any infection, you should avoid visiting vulnerable people, and stay away from school, nursery or work if you are unwell with a fever. Please contact NHS 111 or your GP if you suspect you or your child have scarlet fever – with symptoms such as fever, sore throat, difficulty swallowing and a sandpapery rash. Most illnesses can be managed at home, and NHS.UK has information to help parents look after children with mild illnesses. Contact NHS 111 or your GP surgery if you think your child is getting worse, for instance, if they are feeding or eating less than normal, are dehydrated, have a high temperature that won’t go down, are very hot and sweaty or seem more tired or irritable than normal.
Previous updates
Thursday 20 april 2023.
The latest data from the UK Health Security Agency ( UKHSA ) shows that scarlet fever notifications are in line with what we would generally expect to see at this time of year, and have significantly reduced since the peak in December 2022.
So far this season (from 12 September 2022 to 16 April 2023), there have been 54,394 notifications of scarlet fever. In the last comparable high season (from September 2017 to September 2018), there were 30,768 scarlet fever notifications overall across the year.
While invasive group A streptococcus ( iGAS ) is still a very rare infection, notifications are slightly higher than we would expect at this time of year and remain relatively high in children compared to what we typically see. As in previous seasons, the majority of iGAS cases have continued to be among those aged over 45 years, particularly in those aged over 75 years.
- 2,965 iGAS cases across all age groups, compared to 2,898 across the whole of the last comparably high season in 2017 to 2018
- 701 iGAS cases in children aged 18 years and under, compared to 205 cases in the 2017 to 2018 season
Sadly, so far this season, there have been 401 deaths (from any cause recorded within 7 days of an iGAS infection diagnosis) across all age groups in England. This figure includes 47 children aged under 18 years in England. In the September 2017 to September 2018 season, there were 354 deaths in total across the season, including 27 deaths among children aged under 18 years.
Thursday 30 March 2023
The latest data from the UK Health Security Agency ( UKHSA ) shows that scarlet fever notifications are in line with what we would expect to see at this time of year, and have significantly reduced since the peak in December 2022. However, iGAS notifications remain higher than normally seen at this point in the season.
High levels of iGAS activity at such an early point in the season remains a concern, with further increases possible as we move towards the usual peak time of the year for infections. While iGAS is still very rare, notifications are higher than we would expect at this time of year and remain relatively high in children compared to what we typically see.
There continue to be increased notifications in older adult age groups, and as in previous seasons, the majority of iGAS cases have continued to be among those aged over 45 years, particularly in those aged over 75 years.
So far this season (from 12 September 2022 to 26 March 2023), there have been 52,183 notifications of scarlet fever. In the last comparable high season (from September 2017 to September 2018) there were 30,768 scarlet fever notifications overall across the year.
iGAS infections remain rare but are currently higher than expected in a typical year. So far this season, there have been:
- 2,651 iGAS cases across all age groups, compared to 2,898 across the whole of the last comparably high season in 2017 to 2018
- 635 iGAS cases in children aged 18 years and under compared to 205 cases in the 2017 to 2018 season
Sadly, so far this season, there have been 355 deaths across all age groups in England. This figure includes 40 children aged under 18 years in England. In the September 2017 to September 2018 season, there were 354 deaths in total across the season, including 27 deaths among children aged under 18 years.
Friday 3 March 2023
The latest data from the UK Health Security Agency ( UKHSA ) shows that scarlet fever infections and invasive group A streptococcus ( iGAS ) infections remain high, although they have significantly reduced since the peak in December 2022.
High levels of activity at such an early point in the season remains a concern, with further increases possible in the coming weeks as we move towards the usual peak time of the year for infections. While iGAS is still very rare, notifications remain relatively high in children compared to what we typically see – these rates are more in keeping with the previous high season of 2017 to 2018.
There continue to be increased notifications in older adult age groups, and as in previous seasons, the majority of iGAS cases have continued to be among those aged over 45 years, particularly in those aged over 75 years.
So far this season (from 12 September 2022 to 10 March 2023), there have been 49,372 notifications of scarlet fever. In the last comparable high season (from September 2017 to September 2018) there were 30,768 scarlet fever notifications overall across the year.
iGAS infections remain rare but are currently higher than expected in a typical year. So far this season, there have been:
- 2,415 iGAS cases across all age groups, compared to 2,898 across the whole of the last comparably high season in 2017 to 2018
- 575 iGAS cases in children aged 18 years and under compared to 205 cases in the 2017 to 2018 season
Sadly, so far this season, there have been 319 deaths across all age groups in England. This figure includes 40 children aged under 18 years in England. In the September 2017 to September 2018 season, there were 354 deaths in total across the season, including 27 deaths among children aged under 18 years.
The latest data from the UK Health Security Agency ( UKHSA ) shows that scarlet fever infections remain high and are fluctuating with levels similar to those seen during the last comparably high season in 2017 to 2018.
The number of weekly notifications of invasive group A strep ( iGAS ) in children has slowed since December 2022. High levels of activity at such an early point in the season remains a concern, with further increases possible in the coming weeks as we move towards the usual peak time of the year for infections. While iGAS is still very rare, notifications remain relatively high in children compared to what we typically see – these rates are more in keeping with the previous high season of 2017 to 2018.
Dr Derren Ready, UKHSA incident director, said:
Scarlet fever notifications have fallen significantly since the peak in December but remain at a high level. This decline should be treated with caution as spring is usually the period of the year that we could see infections rise again. Please contact NHS 111 or your GP if you suspect you or your child have scarlet fever – with symptoms such as fever, sore throat, difficulty swallowing and a sandpapery rash. Most winter illnesses can be managed at home, and NHS.UK has information to help parents look after children with mild illnesses. Contact NHS 111 or your GP surgery if you think your child is getting worse, for instance, if they are feeding or eating less than normal, are dehydrated, have a high temperature that won’t go down, are very hot and sweaty or seem more tired or irritable than normal. It is important that we continue to help stop the spread of all germs in the community and to vulnerable groups. Wash your hands regularly and thoroughly, catch coughs and sneezes in a tissue, and keep your home well ventilated. If you are unwell with any infection, you should avoid visiting vulnerable people, and stay away from school, nursery or work if you are unwell with a fever.
So far this season (from 12 September 2022 to 28 February 2023), there have been 47,084 notifications of scarlet fever. In the last comparable high season of 2017 to 2018 (September to September), there were 30,768 scarlet fever notifications overall across the year.
Invasive group A strep infections remain rare but are currently higher than expected in a typical year. So far this season, there have been:
- 2,178 iGAS cases across all age groups, compared to 2,898 across the whole of the last comparably high season in 2017 to 2018
- 242 iGAS cases in children aged 1 to 4 years compared to 194 cases in the 2017 to 2018 season
- 160 cases in children aged 5 to 9 years, compared to 112 during the 2017 to 2018 season
Sadly, so far this season, there have been 285 deaths across all age groups in England. This figure includes 35 children under 18 years in England. In the 2017 to 2018 season (September to September), there were 354 deaths in total across the season, including 27 deaths among children under 18 years.
Thursday 16 February 2023
The latest data from the UK Health Security Agency ( UKHSA ) continues to show that scarlet fever infections remain high, although they are now in line with levels seen during the last comparably high season in 2017 to 2018.
The number of weekly notifications of invasive group A strep ( iGAS ) in children has slowed, but there has been a slight increase in recent weeks. While iGAS is still very rare, notifications remain relatively high in children compared to what we typically see, although these rates are more in keeping with the previous high season of 2017 to 2018. In recent weeks, there has been an increase in older adult age groups, and as in previous seasons, the majority of iGAS cases have continued to be among those over the age of 45, particularly in the over 65s.
Dr Derren Ready, Incident Director, UKHSA , said:
Although the number of scarlet fever notifications we are seeing each week has significantly fallen since the peak in December, the bacteria that cause the infection are still circulating at high levels for this time of the year. Please contact NHS 111 or your GP if you suspect you or your child have scarlet fever – with symptoms such as fever, sore throat, difficulty swallowing, and a sandpapery rash. Early treatment of scarlet fever with antibiotics is important to reduce the risk of a more serious infection and transmission to others. After starting antibiotics, children should be excused from school or nursery, and adults should be excused from work for the first 24 hours. Most winter illnesses can be managed at home, and NHS.UK has information to help parents look after children with mild illnesses. Contact NHS 111 or your GP surgery if you think your child is getting worse, for instance, if they are feeding or eating less than normal, are dehydrated, have a high temperature that won’t go down, are very hot and sweaty or seem more tired or irritable than normal. It is important that we continue to help reduce the spread of all infections in the community and to vulnerable groups. Wash your hands regularly and thoroughly, catch coughs and sneezes in a tissue, and where possible keep your home well-ventilated. If you are unwell with any infection, it’s best to avoid visiting vulnerable people, and stay away from school, nursery, or work if you are unwell with a fever.
So far this season (from 12 September to 12 February), there have been 44,478 notifications of scarlet fever. In the last comparable high season of 2017 to 2018 (September to August), there were 30,768 scarlet fever notifications overall across the year.
Invasive group A strep ( iGAS ) infections remain rare but are currently higher than expected in a typical year. So far this season, there have been:
- 2,081 iGAS cases across all age groups, compared to 2,967 across the whole of the last comparably high season in 2017 to 2018
- 233 iGAS cases in children aged 1 to 4 compared to 194 cases in the 2017 to 2018 season
- 156 cases in children aged 5 to 9 years, compared to 117 during the 2017 to 2018 season
Sadly, so far this season, there have been 262 deaths across all age groups in England. This figure includes 32 children under 18 in England. In the 2017 to 2018 season (September to August), there were 354 deaths in total across the season, including 27 deaths among children under 18.
Friday 3 February 2023
The latest data from the UK Health Security Agency ( UKHSA ) continues to show that scarlet fever infections remain high for this time of year. Although the weekly number of notifications has fallen since the peak in December, cases are still fluctuating at a level above what we usually see during this time of the year. UKHSA will continue to closely monitor the incidence rate.
The symptoms of scarlet fever include:
- sore throat
- a rash that feels like sandpaper to the touch
The rash usually develops after 12 to 48 hours, typically on the chest and stomach first, then rapidly spreading to other parts of the body. On white skin, the rash looks pink or red. On brown and black skin, it might be harder to see a colour change, but you can still feel the sandpaper-like texture of the rash and see the raised bumps.
Contact NHS 111 or your GP surgery if you suspect you or your child have scarlet fever so you can be assessed.
The number of weekly notifications of invasive group A strep ( iGAS ) in children has slowed. While iGAS is still very rare, notifications remain relatively high in children compared to what we typically see. There has been a rise in older age groups in recent weeks and as with previous seasons, over recent weeks the majority of iGAS cases continue to be in those aged over 45 years.
Dr Sarah Anderson at UKHSA said:
Although the number of scarlet fever notifications we are seeing each week has significantly fallen since the peak in December, the bacteria that cause the infection are still circulating at high levels for this time of the year. Please contact NHS 111 or your GP if you suspect you or your child have scarlet fever – with symptoms such as fever, sore throat, difficulty swallowing and a sandpapery rash. Early treatment of scarlet fever with antibiotics is important to reduce the risk of a more serious infection and transmission to others. Children should stay off school or nursery and adults should stay off work for 24 hours after antibiotics have started. Most winter illnesses can be managed at home and NHS.UK has information to help parents look after children with mild illnesses. Contact NHS 111 or your GP surgery if you think your child is getting worse, for instance, if they are feeding or eating less than normal, are dehydrated, have a high temperature that won’t go down, are very hot and sweaty or seem more tired or irritable than normal. It is important that we continue to help stop the spread of all germs in the community and to vulnerable groups. Wash your hands regularly and thoroughly, catch coughs and sneezes in a tissue, and keep your home well-ventilated. If you are unwell with any infection you should avoid visiting vulnerable people, and stay away from school, nursery or work if you are unwell with a fever.
Thursday 19 January 2023
The latest data from the UK Health Security Agency ( UKHSA ) continues to show that scarlet fever infections remain high, although the number of notifications has fallen in recent weeks.
So far this season (from 19 September to 15 January), there have been 38,429 notifications of scarlet fever. In the last comparably high season of 2017 to 2018 (September to August), there were 30,768 scarlet fever notifications overall across the year. There has been a reduction in the weekly number of notifications over the last few weeks, suggesting a decrease in transmission of the bacteria.
Invasive group A strep ( iGAS ) infections remain rare but are currently higher than we see in a typical year. So far this season there have been:
- 1,675 iGAS cases across all age groups, compared to 2,967 across the whole of the last comparably high season in 2017 to 2018
- 190 iGAS cases in children aged 1 to 4 compared to 194 cases in the 2017 to 2018 season
- 132 cases in children aged 5 to 9 years compared to 117 during the 2017 to 2018 season
The number of weekly notifications of iGAS in children has decreased. However, in older age groups, particularly those over 65 years old, infections have not slowed at the same rate and we are monitoring this closely. As with previous seasons, over recent weeks the majority of iGAS cases continue to be in those over 45 years.
Sadly, so far this season there have been 211 deaths across all age groups in England. This figure includes 30 children under 18 in England. In the 2017 to 2018 season (September to August), there were 355 deaths in total across the season, including 27 deaths in children under 18.
Although the number of scarlet fever notifications we are seeing each week is falling, the bacteria that cause the infection are still circulating at high levels. It’s also not unusual to have a dip in the number of cases before the spring, so we could see infections rise again in the coming months. Please contact NHS 111 or your GP if you suspect you or your child have scarlet fever – with symptoms such as fever, sore throat, difficulty swallowing and a sandpapery rash. Early treatment of scarlet fever with antibiotics is important to reduce the risk of a more serious infection and transmission to others. Children should stay off school or nursery and adults should stay off work for 24 hours after antibiotics have started. It’s not too late to take up the free flu and coronavirus (COVID-19) vaccines if you’re eligible – we know that group A streptococcus infections can be more serious when combined with another infection including flu. Most winter illnesses can be managed at home and NHS.UK has information to help parents look after children with mild illnesses. Contact NHS 111 or your GP surgery if you think your child is getting worse, for instance, if they are feeding or eating less than normal, are dehydrated, have a high temperature that won’t go down, are very hot and sweaty or seem more tired or irritable than normal. It is important that we continue to help stop the spread of all germs in the community and to vulnerable groups. Wash your hands regularly and thoroughly, catch coughs and sneezes in a tissue, and keep your home well-ventilated. If you are unwell with any infection you should avoid visiting vulnerable people, and stay away from school, nursery or work if you are unwell with a fever.
Thursday 12 January 2023
Latest data from the UK Health Security Agency ( UKHSA ) continues to show scarlet fever and group A strep ( GAS ) infections remain high, although the number of notifications has fallen in recent weeks.
So far this season (from 19 September to 8 January), there have been 37,068 notifications of scarlet fever. This compares to a total of 4,490 at the same point in the year during the last comparably high season in 2017 to 2018 – although cases in that season started to rise at a different point. In 2017 to 2018, there were 30,768 scarlet fever notifications overall across the year.
Invasive group A strep ( iGAS ) infections remain rare but are currently higher than we see in a typical year. So far this season there have been 1,539 iGAS cases across all age groups, compared to 2,967 across the whole of the last comparably high season in 2017 to 2018. So far this season, there have been 177 iGAS cases in children aged 1 to 4 compared to 194 cases in that age group across the whole of the 2017 to 2018 season.
There have been 128 cases in children aged 5 to 9 years compared to 117 across the whole of the 2017 to 2018 season. As with previous seasons, over recent weeks the majority of iGAS cases continue to be in those over 45 years. There are early indications of an increase of iGAS notifications in the older age groups in recent weeks and we will monitor this trend closely.
Sadly, so far this season there have been 190 deaths across all age groups in England. This figure includes 30 children under 18 in England. In the 2017 to 2018 season, there were 355 deaths in total across the season, including 27 deaths in children under 18.
Dr Sarah Anderson, UKHSA incident director, said:
The number of scarlet fever notifications we are seeing each week has fallen, but we are continuing to monitor the data closely as the school term gets underway, and children mix more. The bacteria that cause scarlet fever are still circulating at high levels so it is important that we continue to do our bit to stop the spread of germs to vulnerable groups, including the elderly by washing our hands regularly and thoroughly, catching coughs and sneezes in a tissue, and keeping our homes well ventilated. It’s not too late to take up the free flu and COVID-19 vaccines if you’re eligible – we know that group A streptococcus infections can be more serious when combined with another infection like flu. Most winter illnesses can be managed at home and NHS.UK has information to help parents look after children with mild illness. Deaths and serious illness following group A strep infection are very rare and the infection can be easily treated with antibiotics. Contact NHS 111 or your GP surgery if you think your child is getting worse, for instance they are feeding or eating less than normal, are dehydrated, have a high temperature that won’t go down, are very hot and sweaty or seem more tired or irritable than normal.
Thursday 5 January 2022
Latest data from the UK Health Security Agency ( UKHSA ) continues to show scarlet fever and group A strep ( GAS ) infections remain high.
So far this season (from 19 September to 1 January) there have been 35,616 notifications of scarlet fever. This compares to a total of 4,192 at the same point in the year during the last comparably high season in 2017 to 2018 – although cases in that season started to rise at a different point. In 2017 to 2018 there were 30,768 scarlet fever notifications overall across the year.
Invasive group A strep ( iGAS ) infections remain rare but are currently higher than we see in a typical year. So far this season, there have been 159 iGAS cases in children aged 1 to 4 compared to 194 cases in that age group across the whole year of the last comparably high season in 2017 to 2018. There have been 118 cases in children aged 5 to 9 years compared to 117 across the whole year of the last comparably high season in 2017 to 2018. The majority of iGAS cases continue to be in those over 45 years.
Sadly, so far this season there have been 151 deaths across all age groups in England. This figure includes 29 children under 18 in England. In the 2017 to 2018 season, there were 355 deaths in total across the season, including 27 deaths in children under 18.
Dr Obaghe Edeghere, UKHSA incident director, said:
As children return to school, scarlet fever and ‘strep throat’ continue to circulate at high levels and so it is important that we all wash our hands regularly and thoroughly and catch coughs and sneezes in a tissue. This will help stop germs spreading between children and to other vulnerable groups and will help prevent the spread of other winter illnesses that are currently circulating at high levels, including flu and COVID-19 . It’s not too late to take up the free flu and COVID-19 vaccines if you’re eligible – we know that group A strep infections can be more serious when combined with another infection like flu. Most winter illnesses can be managed at home and NHS.UK has information to help parents look after children with mild illness. Deaths and serious illness following group A strep infection are very rare and the infection can be easily treated with antibiotics. Speak to a healthcare professional if you think your child is getting worse, for instance they are feeding or eating less than normal, are dehydrated, have a high temperature that won’t go down, are very hot and sweaty or seem more tired or irritable than normal.
Thursday 29 December 2022
Latest data from the UK Health Security Agency ( UKHSA ) continues to show an out of season increase in scarlet fever and group A streptococcus infections and a higher number of cases than seen in a typical year.
So far this season (from 19 September to 25 December) there have been 33,836 notifications of scarlet fever. This compares to a total of 4,672 at the same point in the year during the last comparably high season in 2017 to 2018 – although cases in that season started to rise at a different point. In 2017 to 2018 there were 30,768 scarlet fever notifications overall across the year.
Invasive group A streptococcus ( iGAS ) infections remain rare. So far this season, there have been 151 iGAS cases in children aged 1 to 4 compared to 194 cases in that age group across the whole year of the last comparably high season in 2017 to 2018. There have been 102 cases in children aged 5 to 9 years compared to 117 across the whole year of the last comparably high season in 2017 to 2018. The majority of iGAS cases continue to be in those over 45 years.
Sadly, so far this season there have been 122 deaths across all age groups in England. This figure includes 25 children under 18 in England. In the 2017 to 2018 season, there were 355 deaths in total across the season, including 27 deaths in children under 18.
Dr Obaghe Edeghere, UKHSA incident director, said:
We are continuing to see a rise in scarlet fever and ‘strep throat’ and this is understandably concerning for parents. However I would stress that the condition can be easily treated with antibiotics and it is very rare that a child will go on to become more seriously ill. Over the winter, there are lots of illnesses circulating that can make children unwell and so it is important to avoid contact with other people if you are feeling unwell, wash your hands regularly and thoroughly and catch coughs and sneezes in a tissue. I would also urge all those eligible for free winter vaccines to take advantage of these. Most winter illnesses can be managed at home and NHS.UK has information to help parents look after children with mild illness. However please do make sure you speak to a healthcare professional if you believe your child is getting worse for instance they are feeding or eating less than normal, are dehydrated, has a high temperature that won’t go down, is very hot and sweaty or seems more tired or irritable than normal.
Thursday 22 December 2022
So far this season (from 12 September to 18 December) there have been 27,486 notifications of scarlet fever. This compares to a total of 3,287 at the same point in the year during the last comparably high season in 2017 to 2018 – although cases in that season started to rise at a different point. In 2017 to 2018 there were 30,768 scarlet fever notifications overall across the year.
Invasive group A streptococcus ( iGAS ) infections remain rare. So far this season, there have been 126 iGAS cases in children aged 1 to 4 compared to 194 cases in that age group across the whole year of the last comparably high season in 2017 to 2018. There have been 88 cases in children aged 5 to 9 years compared to 117 across the whole year of the last comparably high season in 2017 to 2018. The majority of iGAS cases continue to be in those over 45 years.
Sadly, so far this season there have been 94 deaths across all age groups in England. This figure includes 21 children under 18 in England. In the 2017 to 2018 season, there were 355 deaths in total across the season, including 27 deaths in children under 18.
Dr Colin Brown, Deputy Director, UKHSA , said:
I understand how this large rise in scarlet fever and ‘strep throat’ may be concerning to parents, however the condition can be easily treated with antibiotics and it is very rare that a child will go on to become more seriously ill. At this time of year, there are lots of winter illnesses circulating that can make children unwell and I would urge all those eligible for free winter vaccines to take advantage of these. Most winter illnesses can be managed at home and NHS.UK has information to help parents look after children with mild illness. NHS services are under huge pressure this winter, but please visit NHS.UK, contact 111 online or your GP surgery if your child has symptoms of scarlet fever or ‘strep throat’ so they can be assessed for treatment.
Thursday 15 December 2022
Latest data from the UK Health Security Agency ( UKHSA ) continues to show an out of season increase in scarlet fever and group A streptococcus infections.
So far this season (from 12 September to 11 December) there have been 7,750 notifications of scarlet fever. This compares to a total of 2,538 at the same point in the year during the last comparably high season in 2017 to 2018 – although cases in that season started to rise at a different point. In 2017 to 2018 there were 30,768 scarlet fever notifications overall across the year.
Invasive group A streptococcus ( iGAS ) infections remain rare. So far this season, there have been 111 iGAS cases in children aged 1 to 4 compared to 194 cases in that age group across the whole year of the last comparably high season* in 2017 to 2018. There have been 74 cases in children aged 5 to 9 years compared to 117 across the whole year of the last comparably high season in 2017 to 2018. The majority of cases continue to be in those over 15 years.
Sadly, so far this season there have been 74 deaths across all age groups in England. This figure includes 16 children under 18 in England. In the 2017 to 2018 season, there were 355 deaths in total across the season, including 27 deaths in children under 18.
*We analyse scarlet fever seasons from week 37 to week 36 the following year. The majority of cases would typically be seen from the beginning of February to April.
Scarlet fever and ‘strep throat’ will make children feel unwell, but can be easily treated with antibiotics. Symptoms to look out for include fever, sore throat, swollen glands, difficulty swallowing, and headache. Scarlet fever causes a sandpapery rash on the body and a swollen tongue. NHS services are under huge pressure this winter, but please visit NHS.UK, contact 111 online or your GP surgery if your child has symptoms of scarlet fever or ‘strep throat’ so they can be assessed for treatment. At this time of year, there are lots of winter illnesses circulating that can make children unwell. Most of these can be managed at home and NHS.UK has information to help parents look after children with mild illness. It is very rare that a child will go on to become more seriously ill, but parents know better than anyone else what your child is usually like, so you’ll know when they are not responding as they would normally. Make sure you speak to a healthcare professional if your child is getting worse after a bout of scarlet fever, a sore throat or respiratory infection – look out for signs such as a fever that won’t go down, dehydration, extreme tiredness, intense muscle pains, difficulty breathing or breathing very fast.
Good hand and respiratory hygiene are important for stopping the spread of many germs. By teaching your child how to wash their hands properly with soap for 20 seconds, using a tissue to catch coughs and sneezes, and keeping away from others when feeling unwell, they will be able to reduce the risk of picking up or spreading infections.
The first symptoms of scarlet fever include flu-like symptoms, including a high temperature, a sore throat and swollen neck glands (a large lump on the side of your neck).
A rash appears 12 to 48 hours later. It looks like small, raised bumps and starts on the chest and tummy, then spreads. The rash makes your skin feel rough, like sandpaper.
On white skin the rash looks pink or red. On brown and black skin it might be harder to see a change in colour, but you can still feel the rash and see the raised bumps.
Contact 111 (online if child over 5) or GP surgery if your child has scarlet fever symptoms.
Symptoms can include nausea and vomiting.
The symptoms of ‘strep’ throat include:
- flu-like symptoms , such as a high temperature, swollen glands or an aching body
Contact 111 (online if child over 5) or GP surgery if your child has ‘strep’ throat symptoms.
The symptoms of iGAS include:
- severe muscle aches
- localised muscle tenderness
- increasing pain, swelling and redness at site of wound
- unexplained diarrhoea or vomiting
There are several viruses circulating that cause sore throats, colds and coughs. These should resolve without needing medical attention. Antibiotics are not needed for viral infections. However, children can on occasion develop a bacterial infection at the same time as a virus and that can make them more unwell.
As a parent, if you feel that your child seems seriously unwell, you should trust your own judgement. Contact NHS 111 (online if child over 5) or your GP surgery if:
- your child is getting worse
- your child is feeding or eating much less than normal
- your child has had a dry nappy for 12 hours or more or shows other signs of dehydration
- your baby is under 3 months and has a temperature of 38°C, or is 3 to 6 months and has a temperature of 39°C or higher
- your baby feels hotter than usual when you touch their back or chest, or feels sweaty
- your child is very tired or irritable
Call 999 or go to A&E if:
- your child is having difficulty breathing – you may notice grunting noises or their tummy sucking under their ribs
- there are pauses when your child breathes
- your child’s skin, tongue or lips are blue
- your child is floppy and will not wake up or stay awake
Cases of GAS usually increase during the winter and the last time significant numbers of cases were reported was in the 2017 to 2018 season. Seasons with high cases can occur every 3 to 4 years but social distancing measures implemented during the coronavirus (COVID-19) pandemic may have interrupted this cycle and may explain the current increase being observed.
While invasive group A strep is rare, close contacts of cases are at greater risk of developing the infection. Health protection teams follow national guidance to manage the contacts of iGAS cases and advise preventative treatment if necessary.
Following an evidence review of individuals who are at greater risk of invasive group A strep, UKHSA has updated guidance to expand the number of vulnerable groups who would be potentially eligible for prophylactic antibiotics following a risk assessment by health protection teams. This evidence review was underway before the current rise in cases, and is now being implemented.
Data published by Public Health Wales and Public Health Scotland is also available.
Thursday 8 December 2022
The latest data from the UK Health Security Agency ( UKHSA ) continue to indicate that there is an out of season increase in scarlet fever and group A strep infections. Cases usually show steepest rises in the new year, but have increased sharply in recent weeks.
So far this season (from 12 September to 4 December) there have been 6,601 notifications of scarlet fever. This compares to a total of 2,538 at the same point in the year during the last comparably high season in 2017 to 2018.
In very rare occasions, the bacteria causing scarlet fever, group A streptococcus ( GAS ) can get into the bloodstream and cause an illness called invasive group A strep ( iGAS ), which can be very serious, particularly in older, younger and more vulnerable groups. iGAS cases across all age groups are slightly higher than expected at this time of year. The latest data continues to highlight a higher proportion of iGAS cases in children than we would normally see. However, iGAS remains uncommon.
So far this season, there have been 85 iGAS cases in children aged 1 to 4 compared to 194 cases in that age group across the whole of the last comparably high season in 2017 to 2018. There have been 60 cases in children aged 5 to 9 compared to 117 across the whole of the last comparably high season in 2017 to 2018. The majority of cases continue to be in those over 45.
Sadly, so far this season there have been 60 deaths across all age groups in England. This figure includes 13 children under 18. In the 2017 to 2018 season, there were 355 deaths in total across the season, including 27 deaths in children under 18.
Cases of GAS usually increase during the winter and the last time significant numbers of cases were reported was in the 2017 to 2018 season. Seasons with high cases can occur every 3 to 4 years but social distancing measures implemented during the coronavirus (COVID-19) pandemic may have interrupted this cycle and explain the current increase being observed.
Currently, there is no evidence that a new strain of GAS is circulating or any increase in antibiotic resistance. Antibiotics are the best treatment and work well against the circulating strains. The increase is likely to reflect increased susceptibility to these infections in children due to low numbers of cases during the pandemic, along with current circulation of respiratory viruses, which may increase the chances of children becoming seriously unwell. However, investigations are under way to understand if there are other factors that could be contributing to the increase this season and to better understand who is currently most affected.
Dr Colin Brown, Deputy Director, UKHSA , said:
Scarlet fever and ‘strep throat’ are common childhood illnesses that can be treated easily with antibiotics. Please visit NHS.UK , contact 111 online or your GP surgery if your child has symptoms of this infection so they can be assessed for treatment. Very rarely, the bacteria can get into the bloodstream and cause more serious illness called invasive group A strep. We know that this is concerning for parents, but I want to stress that while we are seeing an increase in cases in children, this remains very uncommon. There are lots of winter bugs circulating that can make your child feel unwell, that mostly aren’t cause for alarm. However, make sure you talk to a health professional if your child is getting worse after a bout of scarlet fever, a sore throat or respiratory infection – look out for signs such as a fever that won’t go down, dehydration, extreme tiredness and difficulty breathing.
Good hand and respiratory hygiene are important for stopping the spread of many bugs. By teaching your child how to wash their hands properly with soap for 20 seconds, using a tissue to catch coughs and sneezes, and keeping away from others when feeling unwell, they will be able to reduce the risk of picking up or spreading infections.
There are lots of viruses that cause sore throats, colds and coughs circulating. These should resolve without medical intervention. However, children can on occasion develop a bacterial infection on top of a virus and that can make them more unwell. As a parent, if you feel that your child seems seriously unwell, you should trust your own judgement.
Note: We analyse scarlet fever seasons from week 37 to week 36 the following year. The majority of cases would typically be seen from the beginning of February to April.
Friday 2 December 2022
The latest data from the UK Health Security Agency ( UKHSA ) shows that scarlet fever cases continue to remain higher than we would typically see at this time of year.
There were 851 cases reported in week 46 , compared to an average of 186 for the preceding years.
Scarlet fever is usually a mild illness, but it is highly infectious. Therefore, look out for symptoms in your child, which include a sore throat, headache, and fever, along with a fine, pinkish or red body rash with a sandpapery feel. On darker skin, the rash can be more difficult to detect visually but will have a sandpapery feel. Contact NHS 111 or your GP if you suspect your child has scarlet fever, because early treatment of scarlet fever with antibiotics is important to reduce the risk of complications such as pneumonia or a bloodstream infection. If your child has scarlet fever, keep them at home until at least 24 hours after the start of antibiotic treatment to avoid spreading the infection to others.
Scarlet fever is caused by bacteria called group A streptococci. These bacteria also cause other respiratory and skin infections such as strep throat and impetigo.
In very rare occasions, the bacteria can get into the bloodstream and cause an illness called invasive group A strep ( iGAS ). While still uncommon, there has been an increase in invasive group A strep cases this year, particularly in children under 10. There were 2.3 cases per 100,000 children aged 1 to 4 compared to an average of 0.5 in the pre-pandemic seasons (2017 to 2019) and 1.1 cases per 100,000 children aged 5 to 9 compared to the pre-pandemic average of 0.3 (2017 to 2019) at the same time of the year.
So far this season there have been 5 recorded deaths within 7 days of an iGAS diagnosis in children under 10 in England. During the last high season for group A strep infection (2017 to 2018) there were 4 deaths in children under 10 in the equivalent period.
Investigations are also underway following reports of an increase in lower respiratory tract group A strep infections in children over the past few weeks, which have caused severe illness.
Currently, there is no evidence that a new strain is circulating. The increase is most likely related to high amounts of circulating bacteria and social mixing.
There are lots of viruses that cause sore throats, colds and coughs circulating. These should resolve without medical intervention. However, children can on occasion develop a bacterial infection on top of a virus and that can make them more unwell.
As a parent, if you feel that your child seems seriously unwell, you should trust your own judgement. Contact NHS 111 or your GP if:
We are seeing a higher number of cases of group A strep this year than usual. The bacteria usually causes a mild infection producing sore throats or scarlet fever that can be easily treated with antibiotics. In very rare circumstances, this bacteria can get into the bloodstream and cause serious illness – called invasive group A strep ( iGAS ). This is still uncommon; however, it is important that parents are on the lookout for symptoms and see a doctor as quickly as possible so that their child can be treated and we can stop the infection becoming serious. Make sure you talk to a health professional if your child is showing signs of deteriorating after a bout of scarlet fever, a sore throat, or a respiratory infection.
Share this page
The following links open in a new tab
- Share on Facebook (opens in new tab)
- Share on Twitter (opens in new tab)
Updates to this page
Added latest update.
Updated 2017 to 2018 month range.
Updated information on when to contact NHS 111 or GP in 2 December update.
First published.
Related content
Is this page useful.
- Yes this page is useful
- No this page is not useful
Help us improve GOV.UK
Don’t include personal or financial information like your National Insurance number or credit card details.
To help us improve GOV.UK, we’d like to know more about your visit today. Please fill in this survey (opens in a new tab) .
NIHR-funded calculator uses NHS data to predict patients’ risk of falling
- 10 May 2024
Patients’ risk of falling in the next 12 months could be predicted from their NHS data. This has been made possible by a new calculator developed with funding from NIHR.
eFalls is a falls prediction model which uses routinely available primary care electronic health record data, the first of its kind in the world. It has been developed and tested by researchers from the University of Leeds, the University of Birmingham, and a team of collaborators. It can be used to help identify people at risk of hospitalisation or emergency department attendance after a fall over the next 12 months. This means these people can be provided with interventions to prevent falls taking place.
A research paper outlining the findings has been published in Age and Ageing . Falls are common among people aged over 65 and can be devastating for people’s personal independence. The risks are multifactorial. They include conditions that affect mobility or balance; medications, and home hazards. A history of falls is the strongest risk factor. The incidence of falls is also projected to rise in line with the global ageing demographic.
Saving doctors and nurses valuable time
The findings help proactive identification of people who are at risk of experiencing a fall in the next 12 months. eFalls uses existing primary care data, reducing the need for intensive clinical falls assessment. This saves doctors and nurses valuable time. Once identified as at risk of falling, people can be referred on to a specialist falls prevention service for assessment and treatment to prevent future falls.
The National Institute for Health and Care Excellence (NICE) estimates that 40% to 60% of falls result in:
- major lacerations
- traumatic brain injuries
Other complications of falls include:
- loss of self-confidence
- reduced quality of life
- loss of independence
Principal Investigator Andrew Clegg, Professor of Geriatric Medicine in the University of Leeds School of Medicine, said: “Falls are a global health problem of major importance to health and social care systems. Currently, people’s fall risk is usually only assessed when they have already experienced a fall, which means that they might have already experienced a major injury such as a hip fracture. Our eFalls calculator means that, for the first time, it is possible to proactively identify a person’s risk of future falls which means that they can be referred to specialist falls prevention services, reducing the risk of a fall from happening. The ability to put plans in place to protect those at risk is invaluable to the patient and their loved ones.
“The benefit to the health service is that it reduces the need for treatment and care in hospital and in the community, and the associated costs to the NHS of that treatment. We hope that eFalls will be widely adopted across the NHS to prevent falls from taking place.”
Lead author Lucinda Archer, Assistant Professor in Biostatistics at the University of Birmingham, said:
“The eFalls calculator can be used to predict a person’s risk of a fall, based on information that is already included in their GP records. The accuracy of the tool has been thoroughly tested in two large datasets, containing routinely recorded information on patients from Wales and England, which has shown promising results.
“If this accuracy is consistent across the wider population, the use of eFalls to target those who would benefit from specialist assessment could vastly improve the way that falls prevention services are provided in the UK.”
Health Minister Andrew Stephenson said: “Suffering from a fall can be traumatic for both the individual and their family but innovations such as eFalls could provide a fantastic solution to prevent such incidents, saving people from a lot of pain, as well as time and resource for the NHS.
“Our ongoing work to ensure people get the right care at the right time includes giving people access to local falls services and rehabilitations services, but I’m proud that the UK is at the forefront of developing further solutions to such a widespread issue, through co-funding the development of this technology.”
The team set out to produce and assess a robust and reliable method to proactively identify people for falls prevention interventions, due to the currently limited availability of such systems.
The team developed the eFalls tool using data from more than 750,000 healthcare records. Of these almost 35,000 people experienced a fall or a fracture resulting in A&E attendance or hospitalisation within 12 months.
The researchers hope the eFalls prediction model will be successfully integrated into UK primary care electronic patient record systems. They are keen to work with UK policymakers to explore how eFalls could be used to inform health policy.
The eFalls study has been funded by NIHR’s Health Technology Assessment (HTA) Programme . For more information, please visit the study’s web page .
Share this page
Latest news.

New findings on the use of molnupiravir to treat COVID-19

New funding opportunities for novel brain tumour research launched

ADHD digital test approved for use by the NHS
- South Africa
- Czech Republic
- Netherlands
- United Kingdom
- Guest Posts
- Travel Ramblings
Russia: One Week Itinerary
Russia , the largest country in the world has been on my bucketlist for the longest time. This is where the first ‘women only’ tour of Ticking the Bucketlist is headed. We are off tomorrow and would be spending one week in this enchanting land!
Here is what our ‘one week in Russia’ itinerary looks like….
Day 1: Moscow – Izmailovsky Flea Market and ‘Moscow by Night’
We start our trip from Delhi on an Aeroflot flight and reach Moscow at about 0835 in the morning. We head straight to our hotel to stretch our legs and get some shut-eye. We need to charge our batteries for the Russian sojourn. We are staying in the Best Western Vega at the Izmailovsky area, which is very famous for its local flea market. The Izmailovsky Market is the best place in Moscow for souvenir shopping …dolls, porcelain, jewelry boxes…we will buy them all from here.
Day 2: Moscow – Moscow City Tour and Kremlin Tour
A red building at the Red Square of the Kremlin
Having seen the city’s light the previous night, it is time to see the city’s colours this morning. We will set off on the Moscow City Tour shows us the highlights of city, starting with the Red Square. This is our day to click a 1000 pictures in front of all the monuments that represent Moscow…St Basil’s Cathedral, the Bolshoi theatre, the Olympic Stadium and the Sparrow Hills.
Exploring the Kremlin
Today is also the day to visit and learn more about the most famous monument in Russia. Kremlin, literally means a fort inside a city. Dynasties built on the site, one century after another and the site came to known as the Kremlin in the 14the century. The walled structure of the Kremlin includes palaces and cathedrals… and a historical past!
Later in the evening, we will enjoy the Russian circus that many of us have seen to television ever so often. Acrobats, clowns and animals….its is time to let the little girl in you come out and clap her hands!
Day 3: Moscow – Metro Stations and Arbat Street followed by the Bolshoi Ballet
Mosaics on the walls of the metro station
Today, we set out to explore the metro stations of Moscow, each of which is a stellar work of art. Stunning frescos and chandeliers in marble surroundings… it’s a work of art! We will then walk along the Arbat street, which is the city’s only pedestrian street, lined with shops and cafes.
As the night unfolds, I intend to don a classy dress and get set to watch one of the finest shows on earth at the Bolshoi Theatre. I have always been awestruck by the art form and would love to see some of the best performers in the world move gracefully. A performance that is rated as one of the best in the world has to be ticked off my bucketlist!
Day 4: Moscow – Day Tour to Sergiev Posad followed by a crazy bar hopping night!
Sergiev Posad is one the strongest spiritual centres in Russia. Home to stunning churches, Sergiev Posad will give us a flavour of the famous ‘Golden Ring’ of Russia. The tour will take 5-7 hours and we will be back at the hotel in second half.
Exploring Sergiev Posad
This will be our last night in Moscow, and we are not going to leave the city without sampling some fine Russian vodka. So, this night is dedicated to bar hopping and pub crawling. Hope to meet some travellers and make new friends.
Day 5: Saint Petersburg – Sapsan train experience to Saint Petersburg and Matryoshka Doll painting class
Saint Petersburg , our next destination, is at least 700 km away from Moscow… and we will zip zap zoom on the Sapsan (the high speed train) to get there in about four hours! The high speed trains are engineering marvels, worth experiencing and we ride this iron horse in the afternoon, reaching St Peterburg in the evening.
As a group, we also join a masterclass to paint our own nested Matryoshka dolls… our own little souvenir to carry and remind us of a fun week in Russia.
With our very own Matryoshka dolls!
Day 6: Saint Petersburg – City Tour and Peterhof Palace
The day starts with a city tour of Saint Petersburg that will give us a peek into what this city has… many bridges, stunning castles, colourful cathedrals and fortresses.
Post lunch, we will head to the Peterhof Palace, also called the Russian Versailles. With spring having set in, the gardens would be green and the fountains will put up a show…I am excited!
Peterhof Palace
Day 7: Saint Petersburg – Hermitage Museum and Shopping
The highlights tour on the previous day will surely make us want to see more of Saint Petersburg…and we will do so by visiting the Hermitage Museum, which is also called the ‘Louvre of Russia’. The Hermitage complex itself is of architectural delight … and the collections have stories to speak which will hopefully, spike our interest enough to make to go back read our history textbooks.
The Hermitage Museum
The rest of the day is totally free to visit any of the other monuments or simply shop … it’s every girl’s favourite sport, isn’t it?
Our last night Russia… Oh Russia!!!! Tonight we will explore the party scene in SPB … or maybe … pack for the next day?
Day 8: Saint Petersburg …Bye Bye Russia
Memories, souvenirs and new friendships… it’s time take them all back to India! We check out of our hotel and take the flight from SPB to Delhi, via Moscow.
Farewell Russia!
You may also like
About post author, 11 responses.
Your photos are beautiful! I have always wanted to visit Russia, especially after seeing Anastasia (the Disney movie) 🙂 I can’t believe those mosaics are on the walls at the METRO STATION! How unreal. Great stuff, thanks for sharing.
Wow that is quite an awesome itinerary. I mean… huge Russia in 1 week. I am still dreaming of St. Petersbourg. So many people told me that it is gorgeous. And I would die to see the Ballet
You know I have never considered Russia but this itinerary looks amazing. St. Petersburg looks beautiful. I will certainly consider a trip there now
I’ve only been to St Petersburg so far, and did a few tours in the city and around. But I have a good friend in Moscow, so the incentive is definitely there to go back. I enjoy doing those by night experiences and see how cities transform in different times of day – especially if it’s topped with a circus visit, amazing 🙂
We are thinking of heading to Russia next Summer so will deffo use this itinerary, looks amazing! Would love to visit the Kremlin in Moscow! Thanks for sharing!
I have always been fascinated by Russia. I like the colourful rounds domes on the Palaces just like an Aladin’s Palace. FIFA Football World will be held in Russia next year and I will try my best to visit this beautiful country and will follow your itinerary and contact you. 🙂
Moscow and Kremlin city tour looks amazing. Your one week itinerary is helpful and complete tour of Russian delights. St.Petersburg city tour is also enchanting and splendid. I really want to have Russian vacation now after seeing your pictures
Wow, this is awesome. Well weaved itinerary! We had always dreamed of taking pictures of those onion-domed palaces and those colors on the palaces are just mind blowing. We didn’t know that there is a Versailles in Russia the exterior paint and the colors look much similar. We had loved it in France and would love to visit it in Russia too.
The Peterhof Palace is a delight to visit. Highly recommend it if you are in SPB
I haven’t visited Russia, but it’s definitely on the list! This a great itinerary, I love how you included things to do but also gave some leeway to do things on your own as well (like shopping haha). Beautiful pictures, the buildings and Russian dolls are stunning! I wonder if they’re all hand painted.
The dolls are all hand painted. The cost increases depending on the quality of work and the artist.
Leave a Reply Cancel Reply
Save my name, email, and website in this browser for the next time I comment.
Currently you have JavaScript disabled. In order to post comments, please make sure JavaScript and Cookies are enabled, and reload the page. Click here for instructions on how to enable JavaScript in your browser.
Let’s Travel
Your Name (required)
Your Email (required)
Your Message
Download the NHS App or open the NHS website up and login to access a range of NHS services online.
About your NHS App
Find out more about using the NHS App, or the NHS website, to access services online
NHS App help and support
Get help and support with your NHS App
NHS App legal and cookies
Read our terms of use, privacy policy, cookies policy and more
The NHS App is available on iOS and Android:
You can also use the NHS website .
To use the NHS App, you must be aged 13 or over and registered with a GP surgery in England.
Find out more about who can use the NHS App .

IMAGES
COMMENTS
Lines are open 8am-7pm, 365 days a year. We also have specialist advisers at over 120 local Age UKs. Find information about the services your GP can offer you, and what to do if you're too ill to visit your GP, and what services GP practices should offer people aged 75 and over, and people with long-term conditions.
The GP home visit has long been regarded as an integral element of NHS general practice that is needed to support both proactive and reactive care to patients in the community.1,2 There are increasing numbers of people living with multimorbidity and frailty, many of whom have complex healthcare needs and limited levels of social support. Now with the new challenges around providing care at ...
Evening and Saturday appointments. You can see a healthcare professional on: weekday evenings between 6.30pm and 8pm. Saturdays between 9am and 5pm. Call your GP surgery or use their online services to book evening and Saturday appointments. You may be able to get an appointment on the same day. You may be offered an appointment at:
It is recognised good practice for general practices to have systems in place to triage and prioritise home visits. The aim of this alert is to raise awareness of this good practice. Patient safety alerts are shared rapidly with healthcare providers via the Central Alerting System (CAS). Patient safety alerts.
The British Medical Association (BMA) has produced a COVID-19 toolkit for GPs and GP practices. NHS England issued a patient safety alert to raise awareness of the need to have a system in place to assess: whether a home visit is clinically necessary, and. the urgency of need for medical attention. The alert states that:
Home; NHS services; GPs; Back to GPs Find a GP Enter a postcode in England. Search Use your location . We are searching for your location ... Find out more about registering with a GP surgery. How to register with a GP surgery; Registering with a GP surgery outside the area you live; Build Number: 20240923.4. Support links. Home; Health A to Z ...
Once you've chosen a surgery, you'll need to fill in a registration form. These are usually available on: the NHS App. the GP surgery's website. the GP surgery's profile page on the NHS website (Find a GP) You can also get a paper form from the surgery. It's also possible to register with a GP surgery outside your local area.
NHS @home is an approach to providing better connected, more personalised care in people's homes including care homes. It aims to ensure people have faster access to more appropriate and targeted care, without necessarily having to attend emergency care or arrange GP appointments. NHS @home builds upon what we have learned during the COVID-19 ...
At a cost of £233 for an ambulance conveyance and £132 for an ED attendance (source: NHS Reference costs), a primary care-led home visit, if appropriate, is likely to be less costly. The committee concluded that there was no clear evidence to confirm or refute the cost-effectiveness of primary care visits.
Arrange a GP home visit. If you or someone in your family is unable to come to the surgery because of illness, then you can arrange a home visit. You can arrange a visit by using our online form and explaining your problem. We can then arrange to see the most urgent cases first. If you are able to come to the surgery, then we would appreciate ...
There is an increasing use of medical equipment in home settings 3 and with personal health budgets 4 available for some NHS patients, carers will be able to monitor a patient's vital signs with adequate support. Thus, potentially reducing the number of home visits carried out by GPs. ... Home visits with the GP are one of the most ...
The committee noted that urgent home visits would normally be undertaken either by the GP or by a nurse practitioner and accompanied by a dedicated driver from a locally commissioned provider; co-operative of GPs, community NHS Trust or private company. Home visits will generally take about 40-60 minutes (including travel) whereas most surgery ...
According to the NHS website, those who have tried lifestyle changes and have not had any success should see their GP.. The second sign is for those whose snoring has had a 'big impact'. This doesn't just mean for your partner but also for you. Finally, if you feel sleepy during the day or your partner notices you stop breathing during your sleep, then you may have sleep apnoea.
Patients are permitted to change GPs for any reason. It may be something you choose to do because of personal preferences, or after hearing about a specific service offered at a different GP practice. You may also decide to move GPs because the location is more convenient - close to your child's school, or near to your place of work.
With some online health service providers, you can prove who you are online using NHS login. To prove who you are you need to: Take a photo of your ID (passport, UK or EU driving licence, or European national identity card) using your phone. Record a short video of your face while you say 4 numbers, or use your camera to scan your face.
managing requests for home visits, and if any outstanding training needs exist. General practice staff should report all patient safety incidents, including those relating to GP home visits, to the NRLS via the GP eform (or locally established system that uploads to the NRLS): https://report.nrls.nhs.uk/GP_eForm Who: General practices providing
Typically "communication passports" are also available, listing information about a person's health needs and the best ways for NHS staff to communicate with them. Wales Learning disability
Flu season is just around the corner, with those eligible urged to book an appointment for the flu jab. The NHS is rolling out its annual flu vaccination programme this autumn. Those eligible will ...
The GP home visit has long been regarded as an integral element of NHS general practice that is needed to support both proactive and reactive care to patients in the community. 1, 2 There are increasing numbers of people living with multimorbidity and frailty, many of whom have complex healthcare needs and limited levels of social support.
Key points. In the UK, HIV treatment is provided at specialist clinics within the NHS. HIV medications are dispensed at hospital pharmacies or may be provided by home delivery. HIV treatment is provided free of charge, regardless of immigration status. This information is aimed at people who are using the UK National Health Service (NHS), but ...
NHS services are under huge pressure this winter, but please visit NHS.UK, contact 111 online or your GP surgery if your child has symptoms of scarlet fever or 'strep throat' so they can be ...
You can register permanently with some GP surgeries outside your local area. You can also get emergency treatment from a GP surgery for up to 14 days if you're away from home, for example when you're on holiday. If your treatment will last longer than 14 days then you need to register with a GP surgery as a temporary resident.
We hope that eFalls will be widely adopted across the NHS to prevent falls from taking place." Lead author Lucinda Archer, Assistant Professor in Biostatistics at the University of Birmingham, said: "The eFalls calculator can be used to predict a person's risk of a fall, based on information that is already included in their GP records.
Daredevil participants abseiled 14 floors, the height of almost 10 adult giraffes, down the iconic hospital building. They raised a total of £185,000 of essential funds for three charities supporting Guy's and St Thomas' NHS Foundation Trust, helping the hospitals go above and beyond what the NHS can provide.
You can view your GP health record using the NHS App or by logging into your account on the NHS website. You can create an account if you do not already have one. To view your GP record online, you must be: When you create an account, you'll need to prove your identity before you can view your GP health record. This helps keep your record secure.
Today is also the day to visit and learn more about the most famous monument in Russia. Kremlin, literally means a fort inside a city. Dynasties built on the site, one century after another and the site came to known as the Kremlin in the 14the century. The walled structure of the Kremlin includes palaces and cathedrals… and a historical past!
George Pick Aerotours Weekend visit to Moscow - July 2006. Here is Steve Grimshaw's report of our weekend whizz around Moscow in July 2006. (Click on a picture to see a full size image) I've just returned from a long weekend in Moscow which was an interesting experience to say the least.
To use the NHS App, you must be aged 13 or over and registered with a GP surgery in England. Find out more about who can use the NHS App. Download the NHS App, or open the NHS website in a web browser, to set up and log in to your NHS account. Owned and run by the NHS, your NHS account is a simple and secure way to access a range of NHS ...